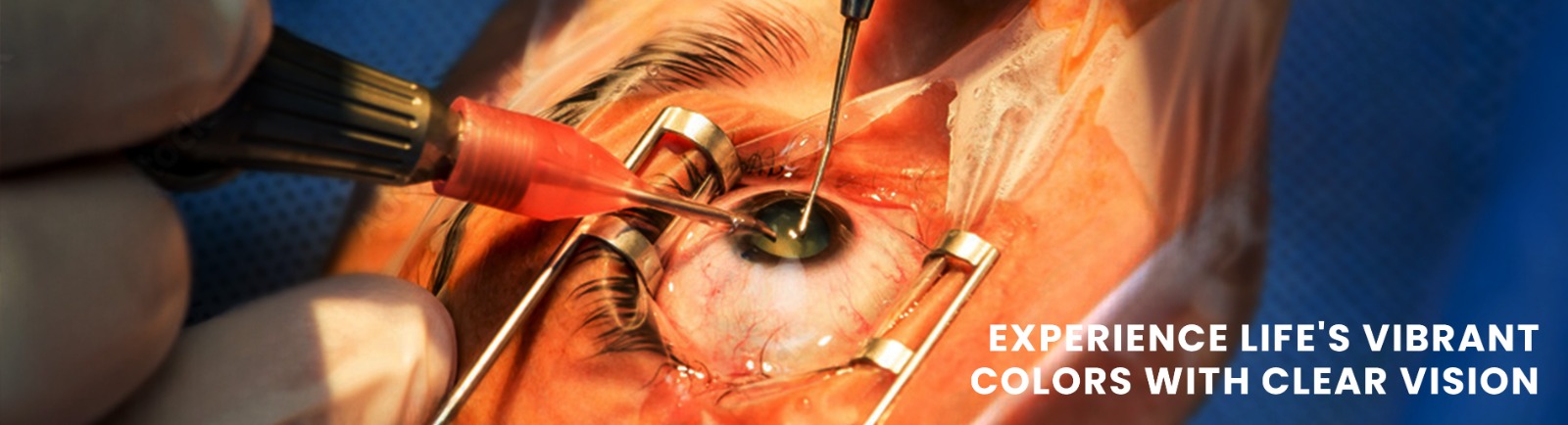
Cataract & IOL Clinic/Service
Do you experience blurry vision? Then you need to immediately consult an eye specialist for a check-up. Cataract is the clouding of the natural eye lens which results in blurry and cloudy vision. Cataract Surgery is the procedure in which cloudy lens is removed and replaced with artificial Intraocular lens (IOL).At Chaithanya, we have specialist doctors having more than two decades of experience in treating cataract in patients of all age group.
How do i make an appointment for this service?
For treatment for urgent and for a routine appointment with our Consultant, you can come directly to, Chaithanya Eye Hospital & Research Institute and is working from Monday to Saturday, 9:00 am – 6:00 pm. For appointments call us at 0471 29 555 00 and our team shall confirm a date & time of your convenience based on the preferred consultant’s day and shall send across the confirmation to your registered mobile no/email, with us.
You can also get information and advice on eye conditions and treatments from our Video Consultation on +91 989 55 999 52. Staffed by experienced ophthalmic surgeons/consultants, the helpline is open from 9am to 6pm, Monday to Saturday. Busy times, we might not be able to answer your call straight away - please bear with us and call back a little later if this happens.
Does Chaithanya provide cashless facility for cataract?
Yes,we do have tie ups with all major insurance providers such as ICICI Lombard, Star Health, Health India, Bajaj Allianz, Future Generali, Religare, Attukal Bhagavathy Trust and other prominent providers too along with CGHS & ECHS. We also have insurance service tie up with major PSU’s such as BSNL, KMML, NIIST & RGCB.
Please feel free to call us on 0471 29 555 00 to know more about insurance services at Chaithanya Eye Hospital & Research Institute.
What do i need to bring with me on the day?
You will need to bring:
All prior records with you in case you are on treatment or have been evaluated for glaucoma in the past.
A list of any medications you are taking.
A list of any eye drops you are taking.
These will be kept in your hospital notes. In addition, please bring your most recent spectacle prescription, or most recent distance and reading glasses.
Do i need to bring someone with me?
Occasionally we need to use eye drops to enlarge the pupil of the eyes so that we can get good quality photographs. These drops can blur your vision for between two to six hours. Thus we advise that you bring someone along on the day of consultation to escort you. After dilatation, you may not be able to drive a vehicle for up to 6 hours.
How many follow up visits are required, does it require a stay over?
In usual cases, 02 follow up visits are required for cataract surgeries. With the surgical expertise and technological advancement, it is a 3-4 hour hospital stay and you are completely fit to go home the same day and nearly 100% functional the very next day after a regular/ routine surgery.
PREPARING FOR CATARACT SURGERY –CHAITHANYA WAY OF EYE CARE Before you come in for your cataract surgery you will need to administer some special eye drops. These drops are very important as they will help to enlarge your pupil so that your doctor can perform the surgery comfortably.
You will be given two different types of eye drops to use prior to surgery.
On the previous day and on the day of the surgery these eye drops have to be used at specified timing which will be informed to you on the day when surgery is fixed.
It is better to have a gap of atleast 10 minutes between use of two different eye drops.
Start by putting one of the drops in the eye to be operated on, and then wait for ONE minute before using the second type of eye drop.
Please remember to wash your hands before you put in your drops.
When you arrive at Chaithanya Eye Hospital, a nurse will check your eyes to make sure you’re ready for surgery and will instill some more eye drops.
For more information and assistance, please call us at 0471 29 555 00.
What to expect on the day of your cataract surgery?
On the day of your cataract surgery
Please arrive promptly, on time at the hospital for your surgery.
You will need to check in at the reception desk when you arrive.
A nurse/ optometrists will welcome and check your details.
You will have some basic observations taken including your temperature, blood pressure and pulse. You will also have your blood sugar level checked if you are diabetic.
A nurse will confirm which eye is being operated on and will mark on your forehead. A doctor will check your eye before surgery and you are shifted to the operation theatre. You will be asked to hand over your belongings to your bystander for safe keeping whilst you are undergoing surgery.
You will be taken to the pre-operative room where you will be looked after by the operation theatre team. They will help you onto the surgery bed where you will be lying flat and monitoring equipment will be connected to check your vital signs during surgery.
Your eyes will be covered with a sterile drape during surgery. Your eye will be anaesthetized so you won’t feel anything during the surgery – this may be by using drops, injection or both.
You may hear sounds of machine during your surgery and may feel water on your eyes. This is all perfectly normal. If you have any discomfort , you are allowed to say it, so that we can help you out.
The surgeon will inform when your operation is finished, which is approximately 10 -20 minutes for cataract procedures.
Your eye will then be dressed with a protective shield. You will be helped off the operation table and staff will take you to the discharge lounge. The nurse in the discharge lounge will take your observations again and check whether you are feeling well enough to leave.
You will be provided with eye drops to use after your operation to help your eye to heal, and instructions on how to look after your eye at home.
You will be seen by the doctor before being discharged.
Once you are happy with your discharge instructions you can go home. Following your surgery, you will also be given an appointment for post–operative review which will be 3 – 5 days after surgery.
How will my eye feel after the operation?
As the effect of the anaesthetic wears off, there can be a dull ache or a foreign body sensation like something in the eye, felt in and around your eye. Your eye may be red, watery and your vision may be blurry.
Your eye usually settles over one to two days after the operation although some patients take slightly longer. A slight feeling of grittiness or as if there is a foreign body in your eye can last for a few weeks after the operation. You should contact us if the pain, redness or blurred vision is getting worse rather than better.
How do i put in the eye drops?
A nurse will teach you how to look after your eye. You will be shown how to clean your eye and put in the eye drops correctly as detailed below.
Tilt your head back.
Gently pull down your lower lid with one hand.
Look up and allow drops to fall inside the lower lid.
Do not let the tip of the bottle come in contact with your eye or fingers.
Wash both hands with soap and water before instilling the eye drops.
In some circumstances, family and friends will be taught how to do this so they can help you.
Is there anything else i must do to care for my eye?
You should avoid rubbing or touching your eye for the first two days after the surgery.
You might find yourself sensitive to light, so it is useful to have a pair of plain dark goggles in case you need them.
The medical and nursing staff will advise you if there are any activities you should avoid.
Most patients can resume normal physical activity within a day or two. You should be able to return to work the day after your first post-operation check up, depending on your occupation.
The doctors and nurses in the clinic will advise you. Your eye will take a couple of weeks to settle and for the best vision to be achieved.
When can i wash my face and hair after the operation?
You are advised to be careful when washing. A Head bath is better avoided till the first post-operation visit to avoid soap and water getting into the operated eye.
A clean face cloth can safely be used. Do not directly splash water into your face in the shower or immerse your head in the bath for one week after surgery.
Please consult our experts to get your eye checkup done and understand what will be best for you. Call us on 0471 2955500 or fill the form on https://www.chaithanya.org/book-an-appointment/ to book an appointment today!
Vitreo Retinal Services Department
Welcome to one of the best Vitreo Retinal Services in South Kerala. At Chaithanya, we strive to provide the best eye care to patients with retinal diseases with the latest and advanced diagnostic tools, medical advice and surgical expertise.

We cater to a wide variety of retinal and choroidal diseases. Retinal diseases include diseases like diabetic retinopathy, hypertensive retinopathy and retinal vascular occlusions which often occur as a consequence of systemic diseases in the body like Diabetes, Hypertension, Cardiac, increased cholesterol, anaemia, etc, acquired retinal diseases like retinal detachments, retinal holes as may be seen often in short-sighted individuals, various infectious and non-infectious diseases of the retina and choroidal layers including manifestations secondary to tuberculosis, sarcoidosis, connective tissue diseases like SLE, acquired macular diseases like age-related macular degeneration, macular holes, macular membranes, macular traction, macular fluid collections like Central Serous Retinopathy (CSR), retinal diseases seen in children and manifestations secondary to blood disorders, drug toxicities and heritable genetic diseases involving the retina.
What are the services offered by Chaithanya under vitreoretinal services?
The Vitreoretinal services at Chaithanya Eye Hospital and Research Institute are located at LEVEL-3 within the new hospital complex. It offers a slew of services including the following
SCREENING PACKAGES
Comprehensive screening for Diabetic eye diseases with a focus on diabetic retinopathy. All diabetic patients need at least one screening session in a year. Do not wait for defective vision to see a doctor. Glass checkups are not enough. If you have not done a ‘dilated examination’ in the past 1 year, Do it today.
Ask for Preclinical diabetic retinopathy screening which includes the state of art, dyeless OCT Angiography which can pick up early manifestations of diabetic retinopathy even before visible on routine angiography or clinical examination.
Age-related macular degeneration screening includes optical coherence tomography and specialized imaging like Blue peak Autofluorescence imaging. If you are 60 years and older, this is the right time for a screening.
Screening for drug toxicity; Patients who are on the following drugs need screening to detect early toxic damage to the retina and optic nerve. Early identification will prevent subsequent loss of vision and will help the treating physician to modify these drugs. Patients on Hydroxychloroquine therapy, antituberculous therapy, antiepileptics, steroids may benefit from this package. Ask your physician whether it is time for screening? Experts advise at least once a year screening for these patients.
ROP Screening for premature and at-risk babies including Retcam imaging. The CRADLE ROP initiative is the only non-public initiative in the state of Kerala which offers screening and care for these newborns. If your baby is born before 8 months and/or had a birth weight of less than 2 kg or needed oxygen therapy in NICU, Talk to the neonatologist and inform us; The CRADLE ROP services will reach your child’s NICU and offer services.
Ocular genetics diseases screening; If there is a family member with a genetic disease involving the eye, do reach us. We offer genetic counselling and advice regarding screening for ocular pathology.
RETINAL DIAGNOSTICS
The Vitreoretinal consultant may advise the following investigations which may be essential for him to make a diagnosis or to rule out other diseases that may closely mimic. The investigations will help the physician to plan the future course of treatment. Some of the investigations may be done the same day, while some may have to do on another day as they may require a physicians consultation before it can be safely done. The following are the diagnostic tests usually done;
Regular fundus camera and scanning laser ophthalmoscope based advanced fundus photography to capture images of the retina. This can be done right away and often needs dilated pupils. The procedure takes less than 5 minutes.
The Heidelberg Spectralis OCT is one of the best optical coherence tomography systems in the world. This german precision equipment provides high-resolution cross section imaging of the retina and dyeless angiography-OCT angiography. This can be done right away and often needs dilated pupils. The OCT procedure takes less than 5 minutes while an OCT Angiography may take 10-15 minutes.
The Heidelberg Spectralis HRA-2 can also perform autofluorescence imaging, infrared photography and perform digital Fundus Fluorescein Angiography (FFA) and Indocyanine Green Angiography (ICG) to carefully study retinal and choroidal circulation problems and detect pathology. FFA/ICG angiography needs dilated pupils and is often planned on a different date because a physician’s fitness is preferably sought before these procedures. Retinal Angiography may take 15-20 minutes
B-Scan/ UBM machine provides digital ultrasound imaging of the inner layers of the eye including specialized anterior segment ultrasonography. This can be done right away and do not need dilated pupils. The procedure takes around 10-15 minutes.
Anterior segment OCT helps to evaluate anterior segment correlating pathology which may be missed in other routine evaluations. This can be done right away and do not need dilated pupils. The procedure takes less than 10 minutes.
Electrophysiological tests; All electrophysiological tests including full-field ERG, pattern ERG, multifocal ERG, EOG, Pattern VEP and flash VEP can be performed to detect heritable diseases and drugs. These procedures may be done on a different date depending on the time slots available on that day for a particular test. The procedure takes anywhere between ½ hour to 1 hour for each test.
MEDICAL RETINA SERVICES
The regular Vitreoretinal outpatient services offer expertise in the diagnosis and treatment of various retinal and choroidal diseases.
The team includes senior consultants and Junior consultants with a wide experience in managing these diseases and have been trained in reputed institutions like Sankara Nethralaya or Aravind Eye Hospital including speciality training abroad.
The following diseases are managed by the medical retina services;
Diabetic retinopathy, hypertensive retinopathy and retinal vascular occlusions often occur as a consequence of systemic diseases in the body like Diabetes, Hypertension, Cardiac, increased cholesterol, anaemia, etc,
Acquired retinal diseases like retinal holes may be seen often in short-sighted individuals.
Various infectious and non-infectious diseases of the retina and choroidal layers including manifestations secondary to tuberculosis, sarcoidosis, connective tissue diseases like SLE, Acquired macular diseases like age-related macular degeneration, other macular bleeding pathologies, macular fluid collections like Central Serous Retinopathy (CSR), Retinal diseases seen in children
Retinal disorders secondary to blood disorders, drug toxicities
Heritable genetic diseases involving the retina.
The Vitreoretinal consultant may advise investigations ( see the section Retinal diagnostics elaborated above) which may be essential for him/her to make a diagnosis or to rule out other diseases that may closely mimic. The investigations will help the doctor to plan the future course of treatment. Some of the investigations may be done the same day, while some may have to do on another day as they may require a general physicians consultation before it can be safely done.
RETINAL LASER THERAPY
The outpatient clinic is equipped with the following laser delivery systems for the management of retinal diseases.
2 IRIDEX laser systems with focal delivery module and indirect laser delivery
IRIDEX Green laser systems with micropulse delivery module
IRIDEX Slit-lamp Transpupillary thermotherapy
PHOTODYNAMIC THERAPY
If you have been advised to have laser therapy for your retinal condition, just call us for a consultation and the procedure can be fixed the same day if the doctor finds it suitable for you.
SURGICAL RETINA SERVICES
Our surgical retina team manages all vitreoretinal surgical conditions and is equipped with one of the best surgical units in the state presently. Chaithanya has been one of the pioneers of vitreoretinal surgery in the state of Kerala especially in the non-government sector and has a round the clock working unit offering surgical expertise for the last 25 years.
Equipped with the latest CONSTELLATION vitrectomy unit with facilities for sutureless small gauge surgery; 23/25/27 gauge instruments, bimanual surgical instruments, dedicated endolaser unit and Cryotherapy.
Surgeons at Chaithanya have access to the latest Leica PROVEO and Zeiss OPMI LUMERA operating microscopes with RESIGHT and BIOM3 wide-angled viewing system.
Surgical conditions managed include; Retinal detachment including complex cases, all Diabetic retinopathy complications requiring surgery, Macular hole, Vitreomacular traction, removal of dislocated lens, intraocular implants, foreign body, management of eye infections; endophthalmitis after surgery or after infections in the body, retinal problems after eye trauma etc. Various retinal diseases in children which require surgery are also managed.
Though most of the above surgical procedures require short term stay (maximum of 1 day overnight) we are a 50 bedded hospital with a full-fledged and equipped inpatient service.
EXPERT CONSULTATIONS
ROP Screening for premature babies: The clinic runs a robust ROP telescreening programme spread over 4 districts in Kerala with NICU based visits on a regular basis. Called the CRADLE ROP initiative, it is one of a kind in the state with RETCAM screening. RETCAM is a wide-angled viewing system used to minimize errors while evaluating these children. We also offer OPD based ROP consultation at the hospital. Feel free to call the CRADLE ROP project at this number for further enquiries. Management of ROP with laser and intravitreal anti-VEGF injections are done here.
Ocular Oncology services: The clinic is also involved in the evaluation and management of eye cancers notably Retinoblastoma which occur in children often by 5 years of age. Retcam based documentation is done and we work in close consultation with Paediatric oncology services at the Regional cancer institute for chemotherapy and radiation therapy and Sri Chitra Thirunal Institute for Medical Sciences and Technology for the latest intraarterial chemotherapy for these eye cancers.
Eye Trauma: Our surgical retina team manages all vitreoretinal surgical conditions related to eye trauma and has a round the clock working unit equipped with one of the best surgical units in the state presently. Trauma in each part of the eye often needs a specialized surgeon managing it and the Chaithanya trauma unit boasts of a highly specialized team of surgeons for optimal results.
Uvea services: The uvea faculty at Chaithanya coordinates a well-organized clinic and offer expertise in the management of uveitis pathology. The service works in close coordination with renowned immunologists and rheumatologists offering steroid-sparing therapy and analyzes tissue fluids and samples which help in arriving at specific aetiological diagnoses of these difficult conditions.
HOW DO I MAKE AN APPOINTMENT TO AVAIL THESE SERVICES?
For a routine appointment with our Consultant, you can call the following number 0471 2955500 and fix an appointment with a consultant. If you wish to choose one of the consultants, the appointment fixing centre will help you to find an appointment slot depending on your convenience and doctor’s availability. The Vitreoretinal services function Monday to Saturday from 9:00 am – 6:00 pm.
This is COVID time and if you are worried to come over to the hospital but would like to get expert advice right away, you can also get information and advice on your eye condition and what you need to do from our Tele Consultation service at +91 989 55 999 52. Staffed by experts, the helpline is open from 9 am to 6 pm, Monday to Saturday.
If you are unable to reach us, just leave a message. We assure you that you will be reached shortly.
If you have an emergency like sudden onset total blindness without any pain or any instance of severe pain with sudden loss of vision, visit our hospital to avail the 24 hr Emergency services. We will take care of your condition. If an expert needs to see you it will be done.
How safe is it, visiting Chaithanya during this pandemic?
Be assured. Chaithanya has taken significant steps to protect the safety and well being of both our staff and patients. We understand that safety is a priority especially during this pandemic.
Before entering Chaithanya Eye Hospital & Research Institute, staff and patients are screened; Potential symptoms of COVID recorded and temperature checked. Everyone must wear a mask at all times in the hospital and masks are provided for patients and accompanies upon arrival. The hospital policy presently allows only one attender to accompany the patient. Dispensers for hand sanitization are located in waiting areas, lifts and throughout all floors. You will find the staff wearing protective clothing. You will also notice that the cleaning staff regularly clean the corridors and examination rooms. Well spaced seating arrangement has been provided. Split waiting area for various examination stations are enforced. A dedicated PRO ensures adequate distancing and monitors safe practices followed by nursing staff. Before you are examined, the relevant instruments are cleaned with antiseptic. The examiner uses antiseptic solution to clean his hands. Protective barriers to avoid aerosol contact is also in place. We have ensured minimum number of people at any given time in a place of examination to maintain social distancing.
Though we offer comprehensive eye care, our outpatient services are distributed across 4 floors with each floor taking care of each speciality to avoid crowding and for the ease of performing the relevant investigations which exists in the same floor. Lift services are available. Walk up to the PRO (You can easily identify these pleasant ladies in their coloured outfits) and ask if you need any help or sort out any issues. Be it queries regarding any delay in examination, payment issues, unhappiness with the staff, fixing appointments or if you are feeling unwell or your sugars are going down, just let them know. They would love to help you.
While we may be following such ideal practices, one needs to understand that this may slow down the various procedures at each station. Please bear with us. Your safety is our primary concern now. Our quality team does a regular audit of cleaning and COVID practices on a daily basis.
Recently we have also altered the scheduling of patients for clinical visits and surgery as per the State Government Covid – 19 protocol norms.
Do i need to carry cash for payment at the hospital?
At Chaithanya eye hospital one can use credit/debit cards for payment. Avail of the facility at the reception on each of the floors. The vitreoretinal service has its own reception at level 3.
Does Chaithanya provides cashless facility for vitreoretinal services?
Yes we do have tie ups with all major insurance providers. This includes PSU on boards, CGHS, ECHS etc. Call us on 0471 29 555 00 to know more about insurance options, insurance facilities and procedures covered.
What should i expect when i go to the retina clinic? How much time will it take to complete my examination?
A comprehensive retinal examination will take atleast an hour. On peak OPD days there could be some variation. The time is variable because some patients may have grave retinal problems where the doctor may have to subject him/her to multiple tests and even get a cross consultation to finalise a diagnosis and institute treatment. At the clinic the following procedures will be done as part of the comprehensive retinal examination:
You need to report at the reception: The reception staff will identify you as a new patient or old patient. New patients often will need a preliminary evaluation before you are worked up for seeing the consultant. Old patients by virtue of the fact they have been to the clinic before and their disease information often loaded into the electronic medical records may bypass this step unless any new additions need to be made. The reception nurse at the reception desk will guide you through this.
Preliminary history taking and data entry: All new patients and certain designated old patients will be seen by an ophthalmologist who will take history from you and record it in the Electronic medical records. Please carry all your old data including investigations and reports and show the doctor during this process. It is a good habit to keep all the old records arranged in chronological order and pinned for easy referral. The doctor will do a basic eye examination using an equipment called slit lamp. Sometimes the doctor may also record your eye pressures in this station.
Visual acuity test: The next step will be getting your vision tested. Sometimes a simple test called the pinhole test will be done which is a very short test. Often a detailed evaluation called refraction is done which could take around 5-10 minutes. This process involves trying out different glass powers so that the best possible power is identified. Sometimes the refractionist will ask you to come back after dilating your eyes to refine the power changes detected. If you need to change your glasses please tell the refractionist at this step. Reading glasses cannot be given after dilatation on the same day. Anyway even though the refractionist finds relevant power glasses for you, the eye doctor will prescribe glasses only after completing his/her examination. Sometimes refractionists would call you for a test called LOW VISION AID Testing which may be done for people with poor reading vision and involves the use of various magnifying glasses and prisms in combination.
Eye pressure test: The next step is eye pressure testing. This is done by the refractionist or an opthalmologist. Numbing drops will be used initially and the test performed. The test may be done with a handheld device (Tonopen) or it may be done on the slit lamp machime with a tonometer(Applanation tonometry).
Dilated eye examination: A good retinal examination needs dilatation of the pupils. Dilating drops are placed in your eyes to widen (dilate) your pupils so that the retina consultant can examine the back of your eyes. Some of the dilating drops used may cause allergy and some are better avoided in certain disease conditions. If you are hypertensive or cardiac, please the nurse. Also if you have allergic to eye drops in the past please inform the nurse. An alternative drug will be used by the nurse in case of the above. Eye allergies due to drops are not serious and may resolve in a few days spontaneously. The usual dilating eye drops would widen your pupils in around 15-20 minutes. The nurse may administer 2-3 drops sometimes to achieve better effect in some individuals. Some of the alternative eye drops may take a longer time. Keep your eye closed after instillation of the drops. It helps in better efficacy of these drugs. Your vision may get blurred after dilatation and may become normal after 2-4 hrs.
Indirect ophthalmoscopy: This test is done by the retina consultant in his/her cabin. Often you may have to lie in a semi-reclined position. The doctor will shine a bright light from the instrument and use a handheld lens to visualize the inner layers of the eyes. He may ask you to look at different directions while examining. He may also use an instrument called ‘Sclera Depressor’ to gently press the eyeball to see certain pathologies clearly. The consultant may also examine you in a seating position on the slit lamp machine using a different set of handheld lenses. All these tests allow the eye care practitioner to identify the disease involving the back of the eye specifically the retina, choroid and optic nerve and plan your treatment.
The Vitreoretinal consultant may advise relevant investigations which may be essential for him to make a diagnosis or to rule out other diseases that may closely mimic. The investigations will help the consultant to plan the future course of treatment. Some of the investigations may be done the same day, while some may have to do on another day as they may require a physician's consultation before it can be safely done( refer to diagnostic services).
Please note that the appointment time given denotes the time when the first examination is done and not the final examination with the consultant.
WANT TO KNOW ABOUT THE LAYOUT OF THE CLINIC. HERE’S AN EYE VIEW
What is an eye angiography?
Angiography of the eye may involve either Fundus fluorescein angiography or Indocyanine angiography or both. Fundus fluorescein angiography is a more common procedure that is performed to give your doctor more information about the condition of the back of your eye especially the retinal circulation. Indocyanine angiography is sometimes performed to give your doctor information about the condition of the choroidal circulation which is a deeper layer of blood vessels in the back of the eye.
In Fundus fluorescein angiography a small amount of yellow fluorescein dye will be injected into a vein in your arm. The dye travels to your eye where it highlights the blood vessels of the retina. It is particularly useful in showing leaking blood vessels and highlighting where the blood supply at the back of the eye is poor. Photographs will then be taken of the eye. The test lasts between 10 to 15 minutes. The results will help your ophthalmologist to decide the best way to treat your eye condition.
In Indocyanine angiography a small amount of Indocyanine green dye will be injected into a vein in your arm. The dye travels to your eye where it highlights the blood vessels of the choroid. It is particularly useful in showing abnormal blood vessels and highlighting where the blood supply is poor. Photographs will then be taken of the eye. The test lasts between 10 to 15 minutes. The results will help your ophthalmologist to decide the best way to treat your eye condition.
Often the two tests are performed together by mixing both the dyes.
Usually, an appointment is given for the procedure. You will often need a physician consultation for fitness. Eye angiography is usually avoided in patients with advanced kidney disease.
If you are given an appointment please report to the reception at the given time. You will not go through the whole process of retinal examination as elaborated above during this visit. You will need to come with a bystander because your eyes will be dilated and may not be able to travel home by yourself.
What happens before the procedure?
Evaluation: The eye doctor and specialist nurse will examine all the medical records that you carry including the fitness documents. They will ask you a few questions regarding your general health and allergy. They will make sure you have been accompanied by a bystander.
Giving consent(permission): We want to involve you in all the decisions about your care and treatment. If you decide to go ahead with the test, you will be asked to sign a consent form that says you have agreed to the treatment and that you understand the benefits, risks and alternatives. If there is anything you don’t understand or you need more time to think about it, please tell the staff caring for you.
Intravenous cannula: A small tube will be placed into a vein in your arm. This is called an intravenous cannula. The fluorescein dye will be injected later through into the bloodstream. Also, this serves as a way to inject medications in case of any allergy later.
Test dose: Fluorescein dye may cause allergy in some individuals. Therefore a diluted form of the drug is tested for drug allergy. A small amount of the drug is injected into the left forearm skin and you will be watched for itching and signs of allergy. FFA procedure will be done only after the allergy testing is negative. Though commonly not as allergic as fluorescein dye, indocyanine green dye is avoided in those with iodine hypersensitivity and advanced renal disease.
Dilatation: You will have eye drops put in to dilate your pupils (make them bigger). The drops will give us a clearer view of the retina at the back of the eye (also known as the fundus).
The Procedure
You will be seated in front of a specialized camera with your chin placed in the chin rest. Please see that you are comfortable in this position. The nurse may hold your head in place.
The fluorescein dye or indocyanine green dye or a mixture of both will then be injected through the venous cannula into the bloodstream. Within seconds, the dye travels through the blood vessels to reach your eye. A series of rapid photographs will then be taken and it is important that you keep as still as possible at this stage. The nurse may help you to keep your eyes open by gently holding your eyelids. You will then be asked to sit back for a few minutes to rest before a further series of photos are taken. The test should take no longer than 15 minutes to complete. Please tell the nurse if you feel unwell at any point. It is common to feel slightly nauseous as the dye goes in, but this passes quickly. Taking deep breaths often helps.
What to expect after the angiography?
After the injection of fluorescein dye, your skin and your urine will turn yellow for approximately 24–48 hours. This is normal and is not harmful and you should not be worried about this. Drinking plenty of water afterwards can help flush the dye through your system. This does not happen with indocyanine green angiography.
Some of the other more common side effects (affecting approximately five people out of 100) include: feeling nauseous or being sick – this usually occurs in the first 1–2 minutes after you are given the injection and in most cases, it will pass within seconds. Taking deep breaths often helps. It is important that you let us know if you have any allergies or if you have had an unexpected reaction to dye before. Very rarely, if the tube becomes displaced and dye leaks into the skin surrounding the tube, you may experience a burning sensation. If this occurs, the injection will be stopped and burning should resolve by itself within a few days. Very rarely, people can have a serious allergic reaction (anaphylaxis) to the dye causing breathing or circulatory difficulties. We are equipped to deal with this emergency and if it happens the emergency medical team will be contacted.
Your doctor may be able to give you the results of the test on the same day and discuss your angiography result and further management.
After the procedure, you will be asked to stay in the department for approximately 30 minutes after the test so that you can be observed for any late side effects. The cannula will then be removed before you go home.
As your pupils will still be dilated (bigger than usual), your eyes will be very sensitive to sunlight for at least two hours. It is advisable to wear sunglasses or a hat to reduce the discomfort.
You must not drive immediately after the procedure and until your pupils return to their normal size. That is why you are advised to bring someone with you to help you get home.
VITREORETINAL LASER PROCEDURE
LASER stands for Light Amplification by Stimulated Emission of Radiation. It is a high energy beam of light which is used to treat the eyes in various ways. LASERs used in the OPD (Outpatient Department) are mainly used for the management of retinal and anterior segment conditions. These are done usually to the swelling in the central part of the retina (Macular oedema), for areas of ischemia in the retina especially when abnormal new vessels are formed or to weak areas in retina (holes, tears).
Laser procedure advised may be done the same day or an appointment given. If you are given an appointment please report at the reception at the given time. You will not go through the whole process of retinal examination during the laser visit. However, the eyes will need to be dilated prior to the treatment.
LASER can be delivered either by indirect ophthalmoscope (LIO) or by slit lamp. LIO is usually preferred if the area to be treated is in the far periphery or when the view of the retina is very hazy due to cataract or bleeding. Sometimes your doctor will place a special contact lens over the eye to control eye movement and direct the laser light precisely. This laser is performed using slit-lamp delivery. Anaesthetic drops are applied before commencing slit lamp delivery of LASER. Retinal laser procedure usually takes about 5-15 minutes.
Most patients have little if any pain following retinal laser surgery. Patients who require more extensive lasers may have an ache inside the eye or around the eye for a few hours. If you have prolonged discomfort after laser take rest and some pain reliever. Please let your doctor know if the pain is severe. You can wash your face or take bath. You can travel but avoid driving yourself if the vision is blurred. Please avoid physical exertion. Reading and watching TV is allowed. You may need to return for more treatments. The number of treatments varies depending on your condition and the doctor will let you know this.
Want to know about lasers that we use?
Green LASER (532nm): This is the conventional form of retinal laser and gives the best result in a clear media. This LASER can be delivered by LIO or by slit lamp. Our hospital has facilities to deliver this LASER through slit lamp as a single spot or multiple spot LASER.
Red LASER (810 nm):
Due to its larger wavelength, the LASER penetrates deeper tissues. It also penetrates better in eyes with retinal haemorrhage, especially in age-related macular degeneration. A special form of this laser delivery is TTT. TTT stands for transpupillary thermotherapy. It is also used for treating ocular tumors.
EYE INJECTIONS FOR RETINAL DISEASES
Eye injections are used to administer medications to treat a variety of retinal conditions. They are called intravitreal injections because they are injected into the vitreous cavity of the eye. The common injections include a group of agents called anti-VEGF agents, steroids and antibiotics. Age-related macular degeneration (AMD), diabetic retinopathy and retinal vein occlusion are the most common conditions treated with intravitreal anti-VEGF drugs. The common intravitreal drugs that we use include Ranibizumab ( LUCENTIS, ACCENTRIX, RAZUMAB), Aflibercept (EYLEA), Brolucizumab ( PAGENAX). Intravitreal steroids like triamcinolone and dexamethasone (OZURDEX) are used in some eyes with diabetic retinopathy, retinal vein occlusion and uveitis. The anti-VEGF drugs and steroids help to reduce fluid leakage associated with these disorders. Intravitreal injections often need to be repeated in conditions such as AMD, diabetic macular edema, and retinal vein occlusions, which require frequent injections. Repeat injections are usually safely tolerated over several years. We do not prefer the use of Bevacizumab (AVASTIN) considering the risk of eye infections with spurious preparations in the market. Safety has been our priority over the years.
The need for an eye injection for a retinal disease is determined during the clinical examination by the retinal physician. Often the retinal physician resorts to investigations like OCT to decide on repeat injections. The nursing staff may advise you to undergo an OCT scan before you visit the doctor after previous injection. Sometimes FFA/ICG angiography or OCT angiography may have to be done.
PREPARING FOR EYE INJECTIONS
Make sure you have met the counsellor at the surgery fixing centre. Make sure you get the date of injection handwritten.
Please confirm if you need any special fitness or approval
Make sure that you understand what drops to use before the surgery.
Before you come in for your injection you will need to administer the eye drops already prescribed.
The drop given is the antibiotic drops that need to be instilled on the day prior to injection and on the morning of injection.
To give the drops enough time to work you need to start using the drop ONE hour before your appointment time on the day of your operation.
Please remember to wash your hands before and after you put in your drops.
The last drop can be administered upon arrival at the hospital.
Once you undergo the procedure you will not be able to travel alone, please make necessary arrangements for your travel to the hospital and back.
For more information and assistance, please call us at 0471 29 555 00.
What to expect on the day of injection?
Please arrive promptly at the hospital for your surgery, at the specified time. Please take care to plan your journey to avoid unexpected traffic and delays.
You will need to check-in at the reception desk when you arrive.
You will be directed to the Injection clinic where the initial preparation is planned.
A nurse/ optometrist will check all the records and the investigations. This includes ocular and other investigations if applicable and fitness documents.
They will ensure that your eyes are sufficiently dilated for the procedure.
You will undergo basic evaluation including recording blood pressure and pulse. You may also have your blood sugar level checked if you are diabetic.
A nurse will confirm which eye is being injected and will mark your forehead with a sticker over the corresponding eyebrow or mark an arrow using a special disposable pen.
A retinal surgeon will meet you and clarify things. The doctor may check your eyes and see you if you have any redness or discharge.
You may have to change into a theatre gown from your street clothes.
You will be asked to hand over your belongings to the bystander for safe keeping whilst you are going for the injection.
You will be taken to the operating room by the assistant. If you need a wheelchair, please ask for one.
What happens in the operating room?
You will be taken to the surgical reception zone. The nursing orderly will confirm the details of injection from the records, perform a quick check on the eye to be injected, investigations are done and provide you with a cap and a protective legging.
She will instil betadine eye drops for sterilising the eye to be operated on.
You will be then shifted into the main operating room.
You will have to lie down flat on the operating table. Monitors may be connected to record your pulse, blood pressure and oxygen concentration.
The surgical nurse and the whole surgical team will confirm with you your name and eye to be injected.
She will then use betadine solution to paint the region of the face and eye that is to be injected. She will also instil local anaesthetic drops and betadine drops into the eye.
She will then cover the eye with a sterile drape
The surgeon takes over from here and performs the injection which would take a few minutes.
You will be conscious and can hear the surgical team talking and the beep of the monitors. Try to stay relaxed. Do not indulge in any unnecessary conversation.
If you have any discomfort or pain, do let the surgical team know about it.
The surgeon will tell you when the procedure is finished. He may also give you some instructions to follow. The instructions will also be shared with you and bystanders later when you reach the room.
Your eye will then be dressed with a protective shield. You will be helped off the trolley and staff will take you to the post-operative zone.
The nurse in the postoperative zone will check if you are feeling well enough to leave the operating theatre complex.
What to expect in the post-injection?
When you reach the inpatient services in your room, the nursing staff will convey the post-operative instructions as directed by the surgeon.
There is no restriction on food to be taken. Diabetics should however take care of maintaining a diabetic diet.
All the previous medications used by the patient can be taken unless specified otherwise.
Patients need to maintain the head position if needed, as specified by the surgeon and nursing staff
The nursing staff will also advise regarding how to clean the eye and share general instructions regarding eye care.
You will be discharged after half an hour of observation. A discharge sheet will be given with all the necessary information. Please refer to the discharge sheet in case of any doubt regarding medications, instructions or follow up visits. The discharge sheet also contains all the relevant information about the procedure done. This document can be used if in need, to see a general physician/ surgeon for other general health problems.
It is normal to feel itching and have sticky eyelids and mild discomfort in the injected eye for a few days. Some people may have redness in the white of the eye which can be ignored. Please don’t rub your eye as this may increase infection and lead to complications.
You can take your bath and face wash after 24 hrs
Your vision may be blurry and the eye will take a few days, usually 2-4 weeks to settle and vision to stabilize.
If you experience severe pain, redness or loss of vision within the first week or later please report back to the hospital the same day. It may be a sign of infection and require different management. Though rare this is a complication that can occur in some predisposed individuals.
Patients who receive OZURDEX implants may see the drug as a linear opacity floating in front of the eye. Patients who receive TRICORT also may see floating particles. It is entirely normal to see this. These patients need to maintain a sitting position for at least 2 hours after the procedure.
Restart all your other medications if you have stopped them unless specified.
You will be given an appointment, usually 30 days after the procedure or later depending on the disease condition. Your next visit may be for an examination or for the next dose of injection.
How do i put in the eye drops?
A nurse will teach you how to look after your eye. You will be shown how to clean your eye and put in the eye drops correctly as detailed below.
Tilt your head back
Gently pull down your lower lid with one hand
Look up and allow drops to fall inside the lower lid
Do not let the tip of the bottle come in contact with your eye
In some circumstances, family and friends will be taught how to do this so they can help you.
PREPARING FOR VITREORETINAL SURGERY
Make sure you have met the counsellor at the surgery fixing centre. Make sure you get the date of surgery handwritten. Sometimes you may have to come to the hospital for an eye injection usually done 3-5 days prior to the surgery. Was it advised for you?
Make sure that you understand what drops to use before the surgery.
Before you come in for your vitreoretinal surgery you will need to administer the eye drops already prescribed. You will be given two different types of drops to be put in.
One of these drops is meant to enlarge the pupil so that your doctor can see into the back of your eye during your surgery.
The other drop is the antibiotic drops that need to be instilled on the day prior to surgery and on the morning of surgery.
To give the drops enough time to work you need to start using the drop ONE hour before your appointment time on the day of your operation. Start by putting one of the drops in the eye to be operated on, and then wait for a few minutes before using the second type of eye drop.
Please remember to wash your hands before and after you put in your drops.
The last drop can be administered upon arrival at the hospital.
Once you put these eye drops in you will not be able to travel alone, please make necessary arrangements for your travel to the hospital and back.
For more information and assistance, please call us at 0471 29 555 00.
What to expect on the day of your surgery?
Please arrive promptly at the hospital for your surgery, at the specified time. Please take care to plan your journey to avoid unexpected traffic and delays.
You will need to check-in at the reception desk when you arrive.
You will be directed to the inpatient services where the initial preparation is planned.
A nurse/ optometrist will check all the records and the investigations. This includes ocular and other investigations like blood tests, ECG, XRAY if applicable and fitness documents.
They will ensure that your eyes are sufficiently dilated for surgery. Additional drops may be instilled if needed. Eyelashes may be clipped in some surgeries.
You will undergo basic evaluation including recording temperature, blood pressure and pulse. You may also have your blood sugar level checked if you are diabetic.
A nurse will confirm which eye is being operated on and will mark your forehead with a sticker over the corresponding eyebrow or mark an arrow using a special disposable pen.
The ward doctor may meet you and clarify things. The ward doctor may see you if you have any redness or discharge as identified by the nurse.
An identification wristband will be provided.
A test dose of the local anaesthetic agent will be given. A small amount of the drug is injected into the left forearm skin and you will be watched for itching and signs of allergy.
You may have to change into a theatre gown from your street clothes.
Please remember to use the restroom as vitreoretinal surgeries may be long and may take 1-2 hrs to complete.
You will be asked to hand over your belongings to the bystander for safekeeping whilst you are undergoing surgery.
You will be taken to the operating room by the assistant. If you need a wheelchair, please ask for one.
What happens in the operating room?
You will be taken to the surgical reception zone. The nursing orderly will confirm the details of surgery from the records, perform a quick check on the eye to be operated, investigations are done and provide you with a cap and a protective legging.
She will instil betadine eye drops for sterilising the eye to be operated on.
You will next be taken to the Anesthetic zone. The anaesthesia assistant will help you onto a trolley, where you will be lying flat.
The anaesthetist will see you here and after a quick evaluation and record perusal prepare you for the ocular anaesthesia.
Initially, an intravenous cannula will be placed in your forearm region or where suitable vein access is possible.
The skin around your eyes will be sterilized with iodine swabs.
Your eye will be anaesthetized with an injection given around the eye. Though this procedure may be painful initially, as soon as the anaesthetic agent works you will feel no pain. The anaesthetist may check your eye movements and may add more injections. He will massage your eyes gently after the local anaesthesia. Please understand that eye surgeries are done under local anaesthesia wherein you will not feel any eye pain but you will be wide awake and can hear the surgeons and nursing assistants while at work.
You will be then be shifted into the main operating room.
You will have to lie down flat on the operating table. Monitors will be connected to record your pulse, blood pressure and oxygen concentration. Oxygen by nasal prongs will be given in addition as your face will be covered by a sterile sheet during surgery. Though you may at first feel a little claustrophobic, you will feel comfortable later on. Taking deep breaths will relieve anxiety and convince you that your breath is not restricted.
The surgical nurse and the whole surgical team will confirm with you your name and eye to be operated on.
She will then use betadine solution to paint the region of the face and eye that is to be operated on. She will also instil betadine drops into the eye.
She will then stick the sterile drape around the eye
The surgeon takes over from here and performs the surgery. The usual surgical time may vary from an hour to 2 hrs.
You will be conscious and can hear the surgical team talking and the hum of the operating machine and the beep of the monitors. Try to stay relaxed and take a short nap. Do not indulge in any unnecessary conversation.
Because the temperature in the operating room needs to be maintained at 21’c you may feel cold. Warmers will be provided if you need them while operating.
If you have any discomfort or pain, do let the surgical team know about it.
The surgeon will tell you when your operation is finished. He may also give you some instructions to follow. The instructions will also be shared with you and bystanders later when you reach the room.
Your eye will then be dressed with a protective shield. You will be helped off the trolley and staff will take you to the post-operative zone.
The nurse in the postoperative zone will monitor your general health parameters and check you are feeling well enough to leave the operating theatre complex.
What to expect in the post-operative phase/ when will you be discharged?
When you reach the inpatient services in your room, the nursing staff will convey the post-operative instructions as directed by the surgeon. This will include how to lie down and what medications to use
The nurse will instil eye drops and oral medications or injections as advised by the surgeon
Some patients may have pain or vomiting in the immediate post-operative period and may need additional medicines or physician consultation.
There is no restriction on food to be taken. Diabetics should however take care of maintaining a diabetic diet.
All the previous medications used by the patient can be taken unless specified otherwise.
Patients need to maintain the head position as specified by the surgeon and nursing staff
The surgeon’s assistant will see the patient the next day morning and check the eye condition and check the eye pressure
The operating surgeon will then see the patient subsequently and advise regarding discharge and medication use. He will give instructions regarding post-operative care, positioning and the next follow up.
The nursing staff will also advise regarding how to use the medications, how to clean the eye, how to maintain position and share general instructions regarding eye care.
The discharge process will be completed in an hour’s time after the doctor sees you.
A discharge sheet will be given with all the necessary information. Please refer to the discharge sheet in case of any doubt regarding medications, instructions or follow up visits. The discharge sheet also contains all the relevant information about the disease condition and surgery done. This document can be used if in need, to see a general physician/ surgeon for other general health problems.
How will my eye feel in the days after the operation and what i start seeing again?
After your operation, we will give you eye drops to reduce any inflammation and to prevent infection. We will explain how and when you should use them.
It is normal to feel itching and have sticky eyelids and mild discomfort (gritty sensation due to the stitches) in the operated eye for five to ten days following retinal detachment surgery. Please don’t rub your eye as this may increase infection and lead to complications.
Your vision may be blurry or dark and the eye will take a few weeks, usually 2-4 weeks to settle and vision to stabilize.
You may see a dark shadow in the lower part of the field in the second and third weeks after surgery if you have undergone surgery with gas injection. It is entirely normal and would go away spontaneously.
Your sight will continue to improve slowly over several months. You will be given corrective glasses later which could improve your vision further.
Your final vision will depend on the nature of your original detached retina. If we diagnose and treat it quickly and successfully, most of your central vision will be restored. If the eye already has poor central vision, when we diagnose a detached retina, we might not be able to restore all of your central sights.
You will be given an appointment, usually seven days after surgery or before depending on the expected post-operative recovery. The next examination after that will be planned usually at 2 weekly intervals.
Usually, no suture removal is necessary. Sometimes loose sutures if applied, may have to be removed
Do i need to maintain any particular posture after surgery?
Your surgeon will advise you if it is necessary for you to posture, and in which position you will need to maintain. Most vitreoretinal surgeries need patients to lie prone- i.e lie on their stomach with chin placed on a pillow. Alternatively, you may be allowed to sit face down. The usual time required is 12-18 hrs in a day. Your surgeon will tell you how strict you will have to be and advise you regarding alternate comfortable positions.
How do i put in the eye drops?
A nurse will teach you how to look after your eye. You will be shown how to clean your eye and put in the eye drops correctly as detailed below.
Tilt your head back
Gently pull down your lower lid with one hand
Look up and allow drops to fall inside the lower lid
Do not let the tip of the bottle come in contact with your eye
In some circumstances, family and friends will be taught how to do this so they can help you.
How should i care after surgery?
You should avoid rubbing or touching your eye.
You might find you are sensitive to light, so it is useful to have a pair of plain dark glasses in case you need them.
Use the ‘plastic green eye shield’ provided during sleep. This protects your eye in the event of an inadvertent tilt of the head on the side of the operated eye.
Avoid washing your face or having a head bath until told so by the surgeon.
Use a clean cloth to wet mop your face taking care to avoid water into the eyes.
Use a separate wet towel to mop your hair.
Avoid shaving for a week.
Avoid strenuous exercises.
The doctor and nursing staff will advise you if there are any activities you should avoid.
Please consult our experts' help in case you have any doubts and don’t forget to get your eye checkup done at the right time. Please feel free to call us in case you have severe pain and redness, headache with vomiting and if your vision which was improving suddenly starts to decrease.
Call us on 0471 2955500 or fill the form on https://www.chaithanya.org/book-an-appointment/ to book an appointment today!
Glaucoma Services
Chaithanya Eye Hospital & Research Institute has years of experience in extinguishing second to none, vision care services. We have with us an impressive panel of eminently qualified eye care specialists who have specialized in caring for all forms of Glaucoma conditions. Our glaucoma department includes the latest equipment to assess structural and functional alterations as a consequence of glaucoma such as Humphrey field analyzer, OCT for retinal nerve fibre layer (RNFL) analysis, optic nerve head (ONH) analysis, ganglion cell layer and retina thickness asymmetry.

IS THERE ANY SYMPTOMS FOR THIS DISEASE.
It is widely known as the silent thief of sight, as there are no symptoms in the initial stages. Typically there are no early symptoms associated with Glaucoma.
SHOULD I GET A GLAUCOMA EVALUATION DONE?
Every individual must have an annual ophthalmic evaluation if they are above the 40 years of age. Also glaucoma screening is a must if there is a family history of Glaucoma, systemic disease such as diabetes/ hypertension, high myopia, history of trauma to the eye and long term steroid use.
ARE THERE DIFFERENT TYPES OF GLAUCOMA?
Yes. Some of them are as follows:-
Primary Open Angle Glaucoma – Open Angle Glaucoma is caused – when the pressure inside the eyes called – intraocular pressure (IOP) – is chronically too high. This high eye pressure damages the optic nerve in the back of the eye, leading to permanent vision loss, over the time. Left untreated this condition can eventually cause blindness.
Angle Closure Glaucoma – This occurs when the structure inside the eye that allows fluids to drain normally from the eye called – (drainage angle) becomes restricted. Narrow drainage angles in the eye increases the risk of the drainage angle becoming blocked, resulting in a significant increase in eye pressure and risk of vision loss.
Normal Tension Glaucoma - Rarely, glaucoma can occur even in an eye with normal IOP. This is called normal-tension glaucoma. The only way to detect normal-tension glaucoma is to have regular comprehensive eye exams by an ophthalmologist. During the exam, your eye doctor will examine your optic nerve, which is visible inside your eyes, to rule out this and all other types of glaucoma.
Congenital Glaucoma - Glaucoma in babies and children under the age of 3 is called congenital or infantile glaucoma. In primary congenital and juvenile glaucoma, the increased internal eye pressure is due to prenatal defects within the eye. These defects are not caused by an underlying condition and are typically in the eye’s drainage system. If the fluid produced inside the eye (aqueous humor) can’t drain properly, fluid builds up and increases the intraocular pressure (IOP).
Secondary Glaucoma - Secondary glaucoma is glaucoma caused by any existing condition that raises internal eye pressure enough to damage the optic nerve. It can be treated both by managing the underlying condition that’s causing the issue and by taking medication or having surgery to lower the eye’s pressure.
Pigmentary Glaucoma – In patients with pigment dispersion syndrome, tiny fragments of pigment from the iris can come free. These tiny pieces of pigment are washed into the eyes drainage system, eventually creating a clogging effect as with exfoliating glaucoma. If the blockage elevates the IOP enough, it can lead to optic nerve damage and glaucoma.
Traumatic Glaucoma - Traumatic glaucoma can develop when an eye injury causes increased IOP. For example, blunt trauma may displace the lens so that there is not enough space for the eye’s fluid to move freely, or it may change the size and shape of the drainage angle. It’s also possible for bleeding from an eye injury to clog the trabecular meshwork in the drainage angle.
Neovascular Glaucoma - Certain conditions, such as diabetes, can significantly affect the blood supply to the eyes. The body often tries to correct this issue by growing new blood vessels in the area; in diabetics, this is called diabetic retinopathy. It can also lead to glaucoma when the vessels grow inside the drainage angle and close it off.
HOW DO I MAKE AN APPOINTMENT WITH THIS SERVICE?
For treatment for urgent and for a routine appointment with our Consultant, you can come directly to, Chaithanya Eye Hospital & Research Institute and is working from Monday to Saturday, 9:00 am – 6:00 pm. For appointments call us at 0471 29 555 00 and our team shall confirm a date & time of your convenience based on the preferred consultant’s day and shall send across the confirmation to your registered mobile no/email, with us.
You can also get information and advice on eye conditions and treatments from our Video Consultation on +91 989 55 999 52. Staffed by experienced ophthalmic surgeons/consultants, the helpline is open from 9am to 6pm, Monday to Saturday. Busy times, we might not be able to answer your call straight away - please bear with us and call back a little later if this happens.
DOES CHAITANYA PROVIDES CASHLESS FACILITY FOR GLAUCOMA SERVICES?
Yes, we do have tie ups with all major insurance providers such as ICICI Lombard, Star Health, Health India, Bajaj Allianz, Future Generali, Religare, Attukal Bhagavathy Trust and other prominent providers too along with CGHS & ECHS. We also have insurance service tie up with major PSUs such as BSNL, KMML, NIIST & RGCB.
Please feel free to call us on 0471 29 555 00 to know more about insurance services at Chaithanya Eye Hospital & Research Institute.
What do i need to bring with me on the day?
You will need to bring:
All prior records with you in case you are on treatment or have been evaluated for Glaucoma in the past.
A list of any medications you are taking.
A list of any eye drops you are taking.
These will be kept in your hospital notes. In addition, please bring your most recent spectacle prescription, or most recent distance and reading glasses.
Do i need to bring someone with me?
Occasionally we need to use eye drops to enlarge the pupil of the eyes so that we can get good quality photographs. These drops can blur your vision for between two and six hours. Thus we advise that you bring someone along on the day of consultation to escort you.
WHAT ALL ARE TESTS FOR GLAUCOMA?
TONOMETRY – It is a test that measures the fluid pressures known as intraocular pressure (IOP), inside your eye. With this test your consultant can evaluate whether or not you may be at risk of Glaucoma. The progression stage of glaucoma and the effectiveness of treatment can be evaluated with this test, in a patient.
THE VISUAL FIELD TEST – Produces a map of your complete vision. The peripheral or side vision (which is affected by Glaucoma) can be measured with the help of this test. The severity of your Glaucoma, Level of Vision Loss, Damage to the vision pathways of the brain and other optic nerve diseases can be determined by the results derived from this test.
PREPARING FOR GLAUCOMA SURGERY –CHAITHANYA WAY OF EYE CARE Before you come in for your glaucoma surgery you will need to administer some special eye drops. These drops are very important as they will help to enlarge their pupil so that your doctor can see into the back of your eye during your surgery.
You will be given two different types of single – dose eye drops to put in.
To give the drops enough time to work you need to start using them ONE hour before your appointment time on the day of your operation.
Start by putting one of the drops in the eye to be operated on, then wait for ONE minute before using the second type of eye drop.
Please remember to wash your hands before and after you put in your drops.
You will need to repeat this process until you have used all the drops. The last drop you can administer upon arrival at the hospital.
Once you put these eye drops in you will not be able to travel alone, please make necessary arrangements for your travel to the hospital and back.
When you arrive at Chaithanya Eye Hospital, a nurse will check your eyes to make sure you’re ready for surgery and may give you some more eye drops.
For more information and assistance, please call us at 0471 29 555 00.
WHAT TO EXPECT ON THE DAY OF YOUR GLAUCOMA SURGERY? On the day of your Glaucoma surgery
Please arrive promptly at the hospital for your surgery, but not more than 15 minutes early.
You will need to check in at the reception desk when you arrive.
A nurse/ optometrists will welcome and check your details. They will also ensure your eyes are sufficiently dilated. Additional drops may be given if needed.
You will have some basic observations taken including your temperature, blood pressure and pulse. You may also have your blood sugar level checked if you are diabetic.
A nurse will confirm which eye or eyes are being operated on, and will mark your forehead with an arrow using special disposable pen. Our surgeon may also briefly meet with you.
You will be asked to hand over your belongs to the by stander for safe keeping whilst you are undergoing surgery.
You will be taken to the anesthetic room where you will be looked after by the theatre team. They will help you onto a trolley, where you will be lying flat and put monitoring equipment on you to check your vital signs during surgery.
The skin around your eyes will be sterilized with iodine swabs. Your eye or eyes will be anaesthetized so you won’t feel anything during operation – this may be using drops, an injection or both.
You will be taken into the theatre on trolley and the theatre team will prepare you for surgery. The cataract procedure will be performed by the surgeon.
You may hear machine noises during your surgery and may feel water on your face. This is all perfectly normal.
The surgeon will tell when your operation is finished, which is approximately 20 – 30 minutes.
Your eye will then be dressed with a protective shield. You will be helped off the trolley and staff will take you to the discharge lounge. The nurse in the discharge lounge will take your observations again and check you are feeling well enough to leave.
You will be provided with eye drops to use after your operation to help your eye to heal, and instructions on how to look after your eye when you look after at home.
Once you are happy with your discharge instructions you can go home. Following your surgery you will also be sent on appointment for post – operative review. This will either take place over the telephone or face – to- face in the hospital.
How will my eye feel after the operation?
As the anesthetic wears off, there can be a dull ache or a sharp pain like something in the eye, felt in and around your eye. Your eye will also be red, watery and your vision may be very blurred.
Your eye usually settles over two to four weeks after the operation although some patients take slightly longer. A slight feeling of grittiness or as if there is a foreign body in your eye can last several months after the operation, as the small wound gradually flattens. You should contact us if the pain, redness or blurred vision is getting worse rather than better.
ARE THERE ANY SIDE EFFECTS FOR THIS SURGERY?
Most side effects are mild, such as soreness, redness and bruising and you should easily recover from these. Below are some more serious possible complications. Please be aware that as long as you are regularly checked in the eye clinic, we should be able to identify and treat any problem quickly.
Infection: if you ever get a red sticky eye with yellow discharge, you need to see an eye doctor as quickly as possible. Infection inside the eye (called endophthalmitis) is very rare, but can cause severe damage. This is treated with antibiotics.
Loose stitches: stitches might become loose and cause your eye to become sore and red. Loose stitches need to be removed, usually in the eye clinic.
Very high or low pressure: the pressure in your eye might go very high or very low in the first few weeks after the operation. This might need treatment with drops, medicine or more surgery.
DOES GLAUCOMA SURGERY WORKS?
A glaucoma surgery usually works and the pressure comes down, although sometimes more than one operation is needed.
How do i put in the eye drops?
A nurse will teach you how to look after your eye. You will be shown how to clean your eye and put in the eye drops correctly as detailed below.
Tilt your head back
Gently pull down your lower lid with one hand
Look up and allow drops to fall inside lower lid
Do not let the tip of the bottle come in contact with your eye
In some circumstances, family and friends will be taught how to do this so they can help you.
IS THERE ANYTHING ELSE I MUST DO TO CARE FOR MY EYE?
If you have undergone any surgery or laser treatment for glaucoma, it is important to understand that these procedures are performed to reduce the intraocular pressure and are an attempt to restore the remaining vision.
Follow the instructions of your doctor and attend follow up examinations as advised
Follow the technique properly while instilling the medication into the eye so that the desired effect of medication is attained.
Regular usage of medications
keeping alarms on your mobile phones will remind you to instil your medications on time
making a simple drug chart in a pocket diary as shown in the figure so that it can be noted and showed to your doctor as well.
If you have any difficulty in instilling the medication or if you have any discomfort after using it, let your doctor know about it.
You may not appreciate a change in vision but never stop the medications without consulting your doctor; this can lead to further vision compromise.
WHEN CAN I WASH MY FACE AND HAIR AFTER THE OPERATION?
You are advised to be careful when washing.
A clean face cloth can safely be used. Do not directly splash water into your face in the shower or immerse your head in the bath for one week after surgery.
Please consult our experts to get your eye checkup done and understand what will be best for you. Call us on 0471 2955500 or fill the form on https://www.chaithanya.org/book-an-appointment/ to book an appointment today!
Cornea & Refractive Services

CATARACT & REFRACTIVE SERVICES AT CHAITHANYA Do you experience blurry vision? Then you need to immediately consult an eye specialist for a check-up. Cataract is the clouding of the natural eye lens which results in blurry and cloudy vision. Cataract Surgery is the procedure in which cloudy lens is removed and replaced with artificial Intraocular lens (IOL).At Chaithanya, we have specialist doctors having more than two decades of experience in treating cataract in patients of all age group.
How do i make an appointment for this service?
For treatment for urgent and for a routine appointment with our Consultant, you can come directly to, Chaithanya Eye Hospital & Research Institute and is working from Monday to Saturday, 9:00 am – 6:00 pm. For appointments call us at 0471 29 555 00 and our team shall confirm a date & time of your convenience based on the preferred consultant’s day and shall send across the confirmation to your registered mobile no/email, with us.
You can also get information and advice on eye conditions and treatments from our Video Consultation on +91 989 55 999 52. Staffed by experienced ophthalmic surgeons/consultants, the helpline is open from 9am to 6pm, Monday to Saturday. Busy times, we might not be able to answer your call straight away - please bear with us and call back a little later if this happens.
Does Chaithanya provide cashless facility for cataract?
Yes,we do have tie ups with all major insurance providers such as ICICI Lombard, Star Health, Health India, Bajaj Allianz, Future Generali, Religare, Attukal Bhagavathy Trust and other prominent providers too along with CGHS & ECHS. We also have insurance service tie up with major PSU’s such as BSNL, KMML, NIIST & RGCB.
Please feel free to call us on 0471 29 555 00 to know more about insurance services at Chaithanya Eye Hospital & Research Institute.
What do i need to bring with me on the day?
You will need to bring:
All prior records with you in case you are on treatment or have been evaluated for glaucoma in the past.
A list of any medications you are taking.
A list of any eye drops you are taking.
These will be kept in your hospital notes. In addition, please bring your most recent spectacle prescription, or most recent distance and reading glasses.
Do i need to bring someone with me?
Occasionally we need to use eye drops to enlarge the pupil of the eyes so that we can get good quality photographs. These drops can blur your vision for between two to six hours. Thus we advise that you bring someone along on the day of consultation to escort you. After dilatation, you may not be able to drive a vehicle for up to 6 hours.
How many follow up visits are required, does it require a stay over?
In usual cases, 02 follow up visits are required for cataract surgeries. With the surgical expertise and technological advancement, it is a 3-4 hour hospital stay and you are completely fit to go home the same day and nearly 100% functional the very next day after a regular/ routine surgery.
PREPARING FOR CATARACT SURGERY –CHAITHANYA WAY OF EYE CARE Before you come in for your cataract surgery you will need to administer some special eye drops. These drops are very important as they will help to enlarge your pupil so that your doctor can perform the surgery comfortably.
You will be given two different types of eye drops to use prior to surgery.
On the previous day and on the day of the surgery these eye drops have to be used at specified timing which will be informed to you on the day when surgery is fixed.
It is better to have a gap of atleast 10 minutes between use of two different eye drops.
Start by putting one of the drops in the eye to be operated on, and then wait for ONE minute before using the second type of eye drop.
Please remember to wash your hands before you put in your drops.
When you arrive at Chaithanya Eye Hospital, a nurse will check your eyes to make sure you’re ready for surgery and will instill some more eye drops.
For more information and assistance, please call us at 0471 29 555 00.
WHAT TO EXPECT ON THE DAY OF YOUR CATARACT SURGERY
On the day of your cataract surgery
Please arrive promptly, on time at the hospital for your surgery.
You will need to check in at the reception desk when you arrive.
A nurse/ optometrists will welcome and check your details.
You will have some basic observations taken including your temperature, blood pressure and pulse. You will also have your blood sugar level checked if you are diabetic.
A nurse will confirm which eye is being operated on and will mark on your forehead. A doctor will check your eye before surgery and you are shifted to the operation theatre. You will be asked to hand over your belongings to your bystander for safe keeping whilst you are undergoing surgery.
You will be taken to the pre-operative room where you will be looked after by the operation theatre team. They will help you onto the surgery bed where you will be lying flat and monitoring equipment will be connected to check your vital signs during surgery.
Your eyes will be covered with a sterile drape during surgery. Your eye will be anaesthetized so you won’t feel anything during the surgery – this may be by using drops, injection or both.
You may hear sounds of machine during your surgery and may feel water on your eyes. This is all perfectly normal. If you have any discomfort , you are allowed to say it, so that we can help you out.
The surgeon will inform when your operation is finished, which is approximately 10 -20 minutes for cataract procedures.
Your eye will then be dressed with a protective shield. You will be helped off the operation table and staff will take you to the discharge lounge. The nurse in the discharge lounge will take your observations again and check whether you are feeling well enough to leave.
You will be provided with eye drops to use after your operation to help your eye to heal, and instructions on how to look after your eye at home.
You will be seen by the doctor before being discharged.
Once you are happy with your discharge instructions you can go home. Following your surgery, you will also be given an appointment for post–operative review which will be 3 – 5 days after surgery.
How will my eye feel after the operation?
As the effect of the anaesthetic wears off, there can be a dull ache or a foreign body sensation like something in the eye, felt in and around your eye. Your eye may be red, watery and your vision may be blurry.
Your eye usually settles over one to two days after the operation although some patients take slightly longer. A slight feeling of grittiness or as if there is a foreign body in your eye can last for a few weeks after the operation. You should contact us if the pain, redness or blurred vision is getting worse rather than better.
How do i put in the eye drops?
A nurse will teach you how to look after your eye. You will be shown how to clean your eye and put in the eye drops correctly as detailed below.
Tilt your head back.
Gently pull down your lower lid with one hand.
Look up and allow drops to fall inside the lower lid.
Do not let the tip of the bottle come in contact with your eye or fingers.
Wash both hands with soap and water before instilling the eye drops.
In some circumstances, family and friends will be taught how to do this so they can help you.
IS THERE ANYTHING ELSE I MUST DO TO CARE FOR MY EYE?
You should avoid rubbing or touching your eye for the first two days after the surgery.
You might find yourself sensitive to light, so it is useful to have a pair of plain dark goggles in case you need them.
The medical and nursing staff will advise you if there are any activities you should avoid.
Most patients can resume normal physical activity within a day or two. You should be able to return to work the day after your first post-operation check up, depending on your occupation.
The doctors and nurses in the clinic will advise you. Your eye will take a couple of weeks to settle and for the best vision to be achieved.
When can i wash my face and hair after the operation?
You are advised to be careful when washing. A Head bath is better avoided till the first post-operation visit to avoid soap and water getting into the operated eye.
A clean face cloth can safely be used. Do not directly splash water into your face in the shower or immerse your head in the bath for one week after surgery.
Please consult our experts to get your eye checkup done and understand what will be best for you. Call us on 0471 2955500 or fill the form on https://www.chaithanya.org/book-an-appointment/ to book an appointment today!
Paediatric Care & Squint Ophthalmology Services Department

Get your kids eye check up done on time
Children are not young adults So complaints and problems related to eye in children need specialised area of expertise to diagnose and treat .Vision impairment in childhood has a dramatic impact on the learning abilities and skill developments of the children The squint and pediatric ophthalmology services at Chaithanya is a department dedicated to early detection and timely management of eye problems in children. Early examination is important to ensure normal visual development Our patients range from newborns to even adults with strabismus. We have an efficacious team of Pediatric consultants who have years of service excellence in child vision care services.
GET YOUR CHILD'S EYE CHECK UP DONE IF ANY OF FOLLOWING SYMPTOMS PRESENT
Poor Eye Contact
Squinting Of Eyes
Drooping Of Eyelid
Shaking Of Eyeball
Difficulty In Seeing Distance watching Tv Closely
Redness/Discharge
Rubbing Of Eyes
Headache
Abnormal Head Posture
During Screen Time /Reading
Redness/watering
Squeezing of eyes
Headache
Frequent blinking
WHICH ARE THE COMMON EYE PROBLEMS?
REFRACTIVE ERROR
SQUINT
AMBLYOPIA OR LAZY EYE
ALLERGIC EYE PROBLEMS
STYE
RETINOPATHY OF PREMATURITY
PAEDIATRIC CATARACT
PAEDIATRIC GLAUCOMA
PAEDIATRIC OCULOPLASTY & LACRIMAL PROBLEMS
WHEN SHOULD I GET AN EYE CHECK UP FOR MY CHILD ?
ALL PRETERM BABIES – within 2 weeks of birth
To rule out ROP
To assess red reflex
6 MONTHS OF AGE , when parents note the following
Squint
Nystagmus
Family history of eye disease
BEFORE 3 YEARS OF AGE /BEFORE ADMISSION TO SCHOOL even if no complaints as unilateral cases will not have any symptoms and detected only during check up to rule out Refractive error
Amblyopia
SERVICES AVAILABLE
Comprehensive paediatric eye care
Squint service all types in children and adult
Orthoptic evaluation
Binocular vision clinic /amblyopia clinic
CVI clinic (CEREBRAL VISUAL IMPAIREMENT)
Hand held slit lamp
Tonopen
Examination under anaesthesia
Electrophysiology under sedation
SQUINT SERVICES
Squint-not a sign of good luck
WHAT IS SQUINT?
Two eyes are aligned in different direction when looking at an object It can
be present at birth or develop later .Any squinting in a child persisting beyond 3
months of age in a child needs consultation.
WHY DOES SQUINT OCCUR?
There are six muscles of eye that control movement of eyeball, brain controls
this eye muscles .Any imbalance in eye muscle coordination causes squint
Reasons Can Be :
Poor vision
Refractive
Nerve or muscle damage
Rarely eye or brain tumour
WHAT ARE THE SYMPTOMS?
Crossed eye
Reduced vision
Abnormal head posture
Double vision
WHY SHOULD SQUINT BE TREATED EARLY?
If not treated early can lead to lazy eye and permanent loss of vision and
binocularity (3D vision)
WHAT ARE THE TREATMENT OPTIONS?
Varies with each individual depends on type and cause of squint
Glass
Patching
Exercises
Prism therapy
Botox injection
SURGERY
CAN ADULT SQUINT BE TREATED?
YES ,there is no age limit for surgical correction but vision restoration possible if
done in young age
ARE THERE ANY SIDE EFFECTS FOR THE SURGERY?
Most squint surgery successfully align your eyes
There can be mild soreness of eyes and redness that last last for few days
Undercorrection or overcorrection
Sometimes double vision that disappear within a week
Uvea Services Department

The department of Uvea at Chaithanya Eye Hospital & Research Institute fortifies with highly adept eye care specialists with advanced ophthalmic diagnostic equipment and a well-equipped clinical laboratory inclusive of ocular microbiology services. We have the highest experts in the field to perform complex cataract and vitreoretinal surgeries that may be required for some patients with uveitis.
UVEITIS refers to a range of conditions that cause inflammation of the pigmented layer of the eye called the uvea.
What are the different types of uveitis?
Anterior Uveitis
Iritis – inflammation of the iris
Cyclitis – inflammation of the ciliary body
Iridocyclitis – inflammation of iris and ciliary body
Intermediate uveitis – inflammation of the jelly-like structure in the eye called the vitreous
Posterior uveitis – Inflammation of the retina & choroid
Panuveitis – Inflammation of anterior and posterior segment
What does it feel like?
Your vision could get blurry. You might have redness, pain, inability to look at light or just floaters. It could come on slowly, or you could just wake up with it one morning. It could be in one or both eyes. Uveitis, per se affects the uvea, the layer providing blood supply and nutrition to different parts of the eye. But there could be associated inflammation of the transparent front part of the eye called the cornea, or the white part called the sclera.
Is it of serious concern?
Uveitis is one of the leading causes of loss of sight among working-age individuals. It may be associated with various conditions like cataracts, glaucoma, retinal detachment and damage to the optic nerve. If left untreated, uveitis can lead to serious consequences including blindness.
What are the uveitis treatment services provided at Chaithanya eye hospital?
The treatment of uveitis includes eye drops, eye injections, oral medicines and retinal lasers depending upon the type and severity of the condition along with the systemic condition of the patient.
How long will i have to take treatment for?
The total duration of the treatment depends on the severity of the disease condition, the response to treatment and the systemic condition of the patient. It may range from weeks to years in some individuals.
Who is under threat for uveitis?
Uveitis can occur in any age group including children, adolescents, middle-aged individuals or the elderly.
Is it the same as pink eye?
Your eye could be pink if you have uveitis. But pink eye, also called conjunctivitis, isn’t the same thing. Pink eye is a common condition you get in the lining of your eye. It’s often brought on by allergies, viruses, or bacteria. Uveitis is rare and happens inside your eye. Only about 38 of every 100,000 people have it.
Is it contagious?
No, it’s not contagious and you don’t have to worry about catching uveitis, from someone.
Should i get a uveitis evaluation done?
Every individual must have an annual ophthalmic evaluation if they are above 40 years of age. If you have constant redness, pain, watering, floaters or decreased vision, it would be ideal to schedule an appointment with the ophthalmologist and get your eyes checked at the earliest. On consultation with our doctors, they can determine the best course of action for your visual needs, ensure the benefits of treatment and help you choose the best treatment for your vision care and improvement.
How do i make an appointment with this service?
For treatment for urgent and for a routine appointment with our consultant, you can come directly to Chaithanya Eye Hospital & Research Institute, working from Monday to Saturday, 9:00 am – 6:00 pm.
You can also get information and advice on eye conditions and treatments from our Video Consultation on +91 989 55 999 52. Staffed by experienced ophthalmic surgeons/consultants, the helpline is open from 9 am to 6 pm, Monday to Saturday. Busy times, we might not be able to answer your call straight away - please bear with us and we shall be calling you back in a while. Please consult our experts to get your eye checkup done and understand what will be best for you. Call us on 0471 2955500 or fill the form on https://www.chaithanya.org/book-an-appointment/ to book an appointment today! Request an Appointment
Orbit & Oculoplasty Department

Ophthalmic plastic and reconstructive surgery combines the precision of ophthalmic microsurgery with plastic and reconstructive surgical principles, allowing for sub specialized care of the eyelids, orbit and lacrimal system. The various procedures offered may be reconstructive, restorative or cosmetic. Each of these categories deals with restoring or enhancing structures as well as function to damaged or malfunctioning adnexal structures.
Services include :
Eyelid repair and reconstruction.
Ptosis repair.
Correction of eyelid malpositions.
Lacrimal surgery
Orbital surgery.
Cosmetic oculoplastic surgery.
TRAUMA
Patients with ocular adnexal trauma often have other significant injuries. Ophthalmic evaluation and treatment is delayed until more serious systemic problems have been addressed. Many of these patients are intoxicated, adding a further degree of complexity. Once attention can be safely directed to the ocular adnexal region, priority should be first given to the preservation of vision. Treatment should be delayed until one can determine that the globes are intact.
EYELID TRAUMA can present as simple or complex lacerations, marginal lacerations, lateral or medial canthal injuries and traumatic levator dehiscence. Surgical repair of adnexal trauma should preserve the eye and vision, maintain function and restore cosmesis. A wound should be closed as soon as possible. However, if the patient is systemically unstable or has life threatening injuries, these should be addressed first. An open globe is treated before soft tissue is repaired.
CANALICULAR lacerations are a commonly missed adnexal injury. The diagnosis of a canalicular laceration is made by either direct visualisation of the cut canaliculus or by probing of the canaliculus.
The most important part of the canalicular repair is placement of a stent across the transected portion of the severed canaliculus. The stent is left in place for 6 weeks.
ORBITAL TRAUMA
Periocular trauma resulting in a floor or medial wall fracture generally occurs with blunt injuries due to flying objects ( ball, fists, elbows ), during motor vehicle accidents or associated with a fall. Orbital fractures requiring repair include those which demonstrate motility restriction and larger fractures. Fractures requiring more urgent repair include those in the paediatric population and also small fractures which incarcerate extraocular muscle tissue. Optimal timing of most fractures is between 5 and 10 days following the injury. Delayed fracture repair may be required in case of traumatic optic neuropathy or internal globe injury.The orbital floor may be approached by the subciliary route or more commonly by the transconjunctival route. Once the entire floor fracture has been visualised, herniated tissue is repositioned into the orbit and an orbital floor implant is placed over the fracture site to prevent prolapse of the orbital contents back into the maxillary sinus. The thickness of the floor implant usually ranges from 0.4 to 0.75 mm.
EYELID MALPOSITIONS
In EPIBLEPHARON, redundant lower eyelid tissue causes the eyelid to rotate towards the cornea. Epiblepharon is generally asymptomatic and tends to resolve as the child gets older, but when corneal irritation and injury is imminent, surgical intervention by excising an ellipse of redundant tissue is warranted.
In ENTROPION, destabilisation of the eyelid position occurs resulting in the inward rotation of the eyelid margin. Wies procedure corrects entropion by creating a permanent scar between the anterior and posterior lamellae of the eyelid with a full thickness transverse blepharotomy combined with rotation sutures. Excessive lid laxity can be corrected by a lateral tarsal suspension.
In TRICHIASIS, lashes will grow with abnormal curvature or direction.
In DISTICHIASIS, lashes grow out of the meibomian gland orifices near the posterior lid margin. Lashes that touch the ocular surface can cause irritation, reflex tearing and abrasion which can lead to ocular surface infections, erosions, scarring with temporary or permanent visual loss. Epilation followed by electrocautery and treatment of any underlying instigating cause is important initial treatment.
Lid splitting and excision techniques are also valuable for recalcitrant patients.
In ECTROPION, the lid margin is displaced outward from the ocular surface. Patients present with symptoms related to ocular or conjunctival exposure, cosmetic deformity and lacrimal dysfunction. In lazy-T technique, medial spindle conjunctival resection is combined with a medial wedge resection to correct the medial ectropion. A lateral tarsal suspension can be performed to further correct the lid laxity.
FACIAL PALSY
Abnormalities of the seventh nerve produce significant issues impacting ocular and facial comfort, protection, function and appearance. Rehabilitation must routinely balance concerns of corneal exposure and ocular protection, eyelid malposition and facial deformity and secondary symptoms such as tearing. The patient’s age, physical and mental capabilities, nature and expected duration of the palsy and physical findings will all dictate the intensity of treatment and timetable for consideration of surgical options. Lubrication with eyedrops and ophthalmic ointment is a cornerstone for treatment of most patients. The patient should be encouraged to use lubricants at a frequency that avoids rather than reacts to ocular irritation. Ointment is generally applied at night to minimise the prolonged exposure while sleeping. Botox injection may help to induce a protective ptosis. Tarsorrhaphy creates an adhesion between the upper and lower eyelids.(on a temporary or permanent basis).This approach narrows the eyelid fissure in a graded fashion both horizontally and vertically, and thus diminishes lagophthalmos, the area of exposure and the surface area exposed to evaporation.
BENIGN ESSENTIAL BLEPHAROSPASM is a debilitating condition of unknown cause characterised by bilateral, involuntary and persistent closure of the eyelids.Botulinum A toxin is the first line therapy for essential blepharospasm. At the initial session, the corrugator, depressor superciliaris and orbicularis muscles are injected.Currently most patients obtain relief from neurotoxin injection alone, but myectomy remains a viable option for nonresponders.
HEMIFACIAL SPASM is characterised by a segmental, typically unilateral myoclonus of facial musculature innervated by cranial nerve VII. Botulinum toxin injection is the mainstay of treatment. Symptomatic improvement is achieved in 95% of patients. Following injection into the involved facial musculature, symptoms typically improve within 3 - 5 days, with maximal improvement 10 - 14 days post-injection.
Average duration of clinical effects is approximately 3 months, with reports varying from 3 to 6+ months. In most patients, oral medications are less effective at ameliorating involuntary facial contractions compared with botulinum toxin therapy and the side effects of oral medications tend to outweigh the symptomatic relief achieved. HFS is a physically, psychologically and socially debilitating disorder that frequently goes unrecognised and therefore untreated. With appropriate treatment , the vast majority of patients achieve long term improvement in quality of life measures.
PTOSIS is a unilateral or bilateral droop of the upper eyelid with the patients head in the full upright position and eyes in primary gaze. Patients often seek medical attention because of the visual obstruction or cosmetic deformity caused by ptotic lids. Ptosis occurs due to congenital deficiency of the muscle fibers or disinsertion of the aponeurosis from the tarsal plate.Suspension of the upper eyelid to
the frontalis muscle complex is the standard technique for the correction of severe ptosis with poor or no levator muscle function. If levator disinsertion has occurred reattachment is necessary. If the levator is still attached but stretched, then resection may be necessary.
BLEPHAROPLASTY - excision of herniated orbital fat with eyelid skin excision may be done to enhance the ptosis correction or for purely cosmetic purposes.
LOWER LID BLEPHAROPLASTY will require additional tarsal suspension and orbicularis suspension to address the lower lid laxity.
BROW PTOSIS - in mild cases, botulinum toxin can be used. Most will require a direct or temporal brow lift.
EYELID AND OCULAR ADNEXAL RECONSTRUCTION
The need for reconstruction usually follows eyelid or ocular adnexal cancer excision or extensive trauma.The goals of reconstructive procedures will be restoration of both the anatomy and the dynamic function of the eyelid, creation of a stable eyelid margin, acceptable vertical eyelid height, adequate eyelid closure and maximum cosmesis and symmetry. Smaller defects can be repaired by direct closure. Moderate defects will require advancement or rotation flaps. Large defects involving the lower eyelid margin require adjacent tissue advancement for repair. One such approach involves the use of a modified tarsoconjunctival flap ( Hughes flap ) taken from the undersurface of the upper eyelid. Large defects involving the upper eyelid margin are most commonly repaired utilising a Cutler-Beard procedure. This technique involves advancing a composite full thickness lower eyelid flap into the upper eyelid defect by passing it posterior to the remaining lower lid margin.
LACRIMAL SURGERY CONGENITAL NASOLACRIMAL DUCT OBSTRUCTION is defined as the failure of drainage of tears down the nasolacrimal system in the neonatal age group, most commonly due to persistence of a membrane inferiorly. 90% will resolve spontaneously by 1 year of age. It is managed conservatively for the first 12 months of life with hydrostatic massage of the lacrimal sac. Antibiotics should only be used to treat active infection and in children with a mucopurulent discharge. Children with persistent symptoms after the age of 12 months should undergo nasolacrimal duct probing . When an initial probing fails, symptoms will redevelop within 4 - 8 weeks. Repeat probing is then recommended.
EPIPHORA ( tearing ) is a common complaint, and the evaluation requires a complete workup that is multifaceted and organised. This will help to correctly localise the area of involvement, diagnose the etiology and develop a treatment plan.
PUNCTAL STENOSIS - isolated stenosis of the lacrimal punctum is a frequent cause of epiphora and is more obvious since it is easily visible. Treatment includes surgical opening by punctoplasty.
CANALICULITIS usually requires surgical intervention in the form of canalicular curettage. Large concretions or stones may require canaliculotomy.
NASOLACRIMAL DUCT OBSTRUCTION is more common in middle- aged females, is often of unknown etiology, and may present with or without dacryocististis.
EXTERNAL DACRYOCYSTORHINOSTOMY attempts to establish a low resistance pathway to drain the tears from the eye to the nasal cavity by converting the lacrimal sac into part of the lateral nasal wall. After the lacrimal fossa is visualised, a small osteotomy is initiated through the lacrimal bone and enlarged to approximately 15 mm in diameter. Nasal mucosal flap is sutured to the lacrimal sac flap and standard Crawford silicone tube can be used to intubate the lacrimal system. Occasionally repeating DCR is necessary. If the patient is debilitated or a lacrimal sac tumour is suspected a dacryocystectomy will suffice, where the lacrimal sac is elevated and reflected out of the lacrimal fossa and excised in its entirety.
ORBITAL DISEASE AND SURGERY
The orbit protects and supports the eye and adnexal structures including the optic nerve, vasculature, extra ocular muscles and lacrimal gland. The goal of orbital evaluation is to identify the nature of the orbital disease and its location. If a specific diagnosis is made and medical treatment is recommended, patient will be followed carefully. However surgical intervention is often necessary for a precise diagnosis. When orbital surgery is required the surgical approach is guided by the goal of the surgery, the location of the disease process and the size of the lesion. If the suspected disease process is treatable, a less invasive orbitotomy for biopsy will be adequate. More invasive approaches are sometimes needed for large malignant lesions requiring a surgical cure. Lastly, orbital exenteration is sometimes needed for aggressive orbital tumours.
ORBITITOMY
Superior and inferior anterior orbital lesions can be accessed through a transconjunctival or transcutaneous approach. Medial orbital lesions can be accessed though a transcutaneous, transconjunctival or transcaruncular approach. Lateral orbitotomy with bone window through a transcutaneous approach provides the best access to the deep orbit. The medial third of the upper eyelid can be incised to gain access to the superomedial orbit and optic nerve.
ORBITAL DECOMPRESSION SURGERY
Is designed to restore the normal volume relationship between the orbital soft tissue and bony volume, thereby reducing orbital pressure, proptosis and, when present, compressive optic neuropathy. Numerous surgical techniques including removal of orbital fat and one or all of the 4 orbital walls are utilised to achieve these goals.
SOCKET SURGERY
Loss of an eye to tumor, trauma or end stage ocular disease is a devastating condition. The psychological trauma to the patient from loss of the eye may be worse than the physical disability in some instances. Since eye contact is such an essential part of human interactions, it is extremely important for the artificial eye patient to maintain a natural, normal appearing prosthetic eye.
If the eye is blind, unsightly and phthisical, but without significant discomfort and with no possibility of an intraocular tumour, the patient may be a candidate for a scleral shell ( a thin ocular prosthesis that fits over the blind eye ). The shell provides a natural appearance and allows the patient to retain their own eye. If the eye is not phthisical, a painted contact lens may help improve the cosmesis of the blind eye. Blind, painful eye and blind, non- painful, disfigured eyes where the ophthalmic history is well known and recent posterior segment examination did not demonstrate any evidence that neoplasm can be managed by enucleation or evisceration. Malignant tumours are the most common indication for orbital exenteration.
Evisceration is removal of the eye’s contents leaving the scleral shell intact.
Enucleation is removal of the eye, leaving the eye muscles and remaining orbital contents intact.
Exenteration is removal of the entire orbital contents, including the eye, extra ocular muscles, fat and connective tissue.
An orbital implant is placed into the socket afterr enucleation or evisceration in almost all cases.In rare patients with severe endophthalmitis, implant placement may be delayed until the tissue swelling settles or gross infection resolves. A prosthesis is generally not fit until at least 6 - 8 weeks after anophthalmic surgery. Artificial eye patients are typically seen again in about 1 month. Following the initial fitting process, periodic visits to the ocularist once or twice per year are recommended to polish the prosthesis to keep it smooth and to check the fit. Refitting the socket with a new prosthesis generally every 5 years will help prevent complications.
THYROID EYE DISEASE
Though most commonly associated with hyperthyroidism, patients of all ages can be affected, either in the euthyroid state or with hypothyroidism. Thyroid eye disease impacts not only visual and social functioning, but also reduces the quality of life. The most common functional and cosmetic
abnormality is exposure to the globe. Excess exposure of the ocular surface results in tear film instability and drying, with corneal erosion.
Patients are counselled against smoking tobacco. Particular care should be exercised in achieving a sustained euthyroid status. Supportive care includes use of lubricating drops or ointment, temporary or permanent punctal occlusion, botulinum A toxin and prismatic correction. Eyelid taping will reduce desiccation of the ocular surface. Treatment during the active, inflammatory phase involves systemic corticosteroids and orbital irradiation.It should be remembered that any surgical procedure performed on patients with thyroid eye disease, whether functional or cosmetic, does not alter the underlying disease process. Surgical intervention to alter eyelid position may involve either tarsorrhaphy to purely improve ocular surface protection or eyelid lengthening procedures to correct eyelid retraction and limit scleral show. Orbital decompression is done during the stable phase of thyroid eye disease when there is a lack of change in clinical measures for an interval of 6 months.
Neuro Ophthalmology Department

Neuro-Ophthalmology is a super specialty that merges the fields of neurology and ophthalmology. Neuro-ophthalmologists are responsible for the diagnosis and management of complex systemic diseases of the nervous system that affect vision, field of vision, eye movements and alignment, as well as pupillary reflexes. Chaithanya Eye Hospital & Research Institute have a dedicated department for Neuro Ophthalmology and our highly experienced doctors make sure that the cause of the problem is identified within a very short period and treated accordingly.
WHEN SHOULD I CONSULT A NEURO-OPHTHALMOLOGIST?
Our team will usually suggest you a consultation in Neuro-Ophthalmology after a comprehensive eye examination, in case you need special care. Often, the symptoms that prompt such a referral include those associated with optic nerve disease or diseases of the visual pathway (the nervous system component that connects the eyes to the brain). Other reasons could be the diseases affecting the pupils of the eye, and certain kinds of squint (especially paralytic). You must also consult a neuro ophthalmologist when there is sudden loss of vision, sudden onset of visual field defects, one has double vision or chronic progression of vision loss etc. A direct appointment with neuro-ophthalmologist can be scheduled if you are referred by neurologist or neurosurgeon for an eye check-up.
COMMON SYMPTOMS THAT REQUIRE ATTENTION
The typical symptoms that could signify a neuro-ophthalmological problem include: Sudden decrease or loss of vision
Sudden transient loss of vision (called transient ischemic attack or eye stroke)
Visual hallucinations
Double vision or diplopia
Intractable headaches
Pupillary abnormalities (sluggish reaction, the difference in size of the pupils)
Sudden onset of difficulties in identifying colors
Inability to tolerate bright light
Visual Field Defects
Squint or strabismus (especially adult onset)
TYPES OF EYE DISEASES TREATED BY A NEURO-OPHTHALMOLOGIST
The common eye diseases that require attention from a neuro-ophthalmologist include:
OPTIC NEUROPATHY
Refers to a damage inflicted on the optic nerve of your eye. This condition is one that gets worse over time when not treated. It is yet another reason why a having a regular eye check up is so important. The types of optic neuropathy are:
OPTIC NEURITIS
It is a condition which presents as a sudden onset loss or decrease in vision due to inflammation of the optic nerve. It can be due to an infection, or an autoimmune response. Optic neuritis is often associated with Multiple Sclerosis(MS) and diagnosed cases of MS need frequent eye check-up.
ISCHEMIC OPTIC NEUROPATHY
Optic neuropathy from obstruction of blood vessels seen in patients with diabetes , high blood pressure, heart diseases etc.
TOXIC OR NUTRITIONAL OPTIC NEUROPATHY
The optic nerve may be damaged due to toxic substances found in tobacco, alcohol or certain medicines like Ethambutol (one of the TB medicine). In fact, the optic nerve damage is often due to lack of nutrients and deficiency of vitamin B-complex and folic acid as well. These diseases also present as progressive decreased vision.
PAPILLEDEMA
Papilledema is characterized by the swelling of the optic nerve head (the part of the optic nerve which can directly be seen by your eye doctor during a retinal evaluation) due to increased pressure from inside the brain. It may be due to life threatening conditions like brain tumors, infections like meningitis, encephalitis, etc which needs prompt diagnosis and treatment. In this condition patients usually have normal vision. Headache associated with or without nausea and vomiting is the main feature.
OPTIC ATROPHY
The loss of some or most of the nerve fibers in the optic nerve due to any of causes mentioned above. It can cause permanent irreversible visual damage.
TRANSIENT VISUAL OBSCURATIONS (TVOs)
TVO s are a type of transient ischemia (TIA) or eye stroke , caused due to decreased blood circulation to the eye caused by neck artery blocks(carotid artery block). Patients have sudden temporary vision loss lasting minutes with complete recovery. But this symptom needs prompt attention, to prevent an impending brain stroke.
SQUINT OR STRABISMUS
A misalignment of the eye, especially when sudden in onset, and associated with double vision is often due to paralysis of one or more of the small muscles of the eye, and is called paralytic strabismus. The eye shows limitations of ocular movement as well.
MYASTHENIA GRAVIS (MG)
MG is a progressive neuromuscular disease which causes progressive muscle weakness, which can involve the eye also and cause progressive droopy eyelids(ptosis).
Focal Dystonias
Movement disorders that affect the eyes and face including hemifacial spasm and blepharospasm
TREATMENT SERVICES AT CHAITHANYA EYE HOSPITAL
We provide comprehensive clinical care for all ages and for a broad spectrum of disorders including:-
Sudden or gradual loss of Vision
Blind Spots
Double Vision
Abnormalities of the pupils
Droopy Eyelids
Abnormal Alignment of the yes
Abnormal Eye Movements
Vision Loss from stroke or tumor
We provide comprehensive, cutting - edge diagnostic testing, including a thorough eye exam, measuring visual acuity, pupil reactivity color vision, field of vision and ocular alignment. We conduct computerized vision field tests (Humphrey’s visual field, HVF) and optical coherence tomography (OCT). The tests advised and treatment suggested will depend on individual case diagnosis.
COMMON TESTS FOR DIAGNOSIS AND MANAGEMENT OF NEURO-OPHTHALMOLOGY DISEASES
A comprehensive eye examination is always the mainstay of the disease diagnosis. In addition to this, your doctor will also advise one or more of these special tests to conclude to plan your treatment. These tests include:
Detailed vision assessment
Evaluation of contrast sensitivity and color vision
Neurological visual fields screening
Electrophysiology tests for optic nerve function and retinal function
Orthoptic evaluation
Evaluation of ocular movements
Ptosis Evaluation
Diplopia charting
Optical coherence tomography(OCT) of the optic nerve head
Imaging studies including CT scan, MRI and MR venogram
Lumbar puncture
TESTS REQUIRED IN NEURO-OPHTHALMOLOGY CASE (One or more tests as per the case may be ordered)
Vision test
Colour vision test
Automated Visual Fields
OCT
VEP, ERG
MRI Brain and Orbit
MR arteriogram or venogram Brain and Neck Vessels
CT Brain and Orbit
CT Angiogram of Brain
Carotid and Vertebral Doppler
Blood tests when required.
COMMON CAUSES OF HEADACHE IN NEURO OPHTHALMOLOGY
Ocular headache may occur due to reduced blood flow or spasms of blood vessels in retina or behind the eye. Regular headache may cause like migraine, tension type headache, vascular headache, Non Vascular Headache , posterior scleritis, optic neuritis, malignant hypertension etc. Headaches are common presentation in ophthalmic clinics. It is important to take a clear detailed history of the headaches/ ocular or facial pain, focusing on its frequency, location, duration, intensity,course, triggers and family history of headaches. It is also important to perform a detailed ophthalmic examination to identify any ocular causes. Most patients would need neuro – imaging and might need further referrals to appropriate medical specialties.
WHY DO STROKE AFFECT VISION
Your vision depends on a healthy eye to receive information and a healthy brain to process that information. The nerves in the eye travel from the eye through the brain to the occipital cortex at the back of the brain allowing you to see. Most strokes affect one side of the brain. Nerves from each eye travel together in the brain, so both eyes are affected. If the right side of your brain is damaged, the left side vision in each eye may be affected. It is rare both sides of the brain to be affected by stroke and thus impact in vision.
How do i make an appointment for this service?
For treatment for urgent and for a routine appointment with our Consultant, you can come directly to, Chaithanya Eye Hospital & Research Institute and is working from Monday to Saturday, 9:00 am – 6:00 pm. For appointments call us at 0471 29 555 00 and our team shall confirm a date & time of your convenience based on the preferred consultant’s day and shall send across the confirmation to your registered mobile no/email, with us.
You can also get information and advice on eye conditions and treatments from our Video Consultation on +91 989 55 999 52. Staffed by experienced ophthalmic surgeons/consultants, the helpline is open from 9am to 6pm, Monday to Saturday. Busy times, we might not be able to answer your call straight away - please bear with us and call back a little later if this happens.
Ocular Oncology Department
We, at Chaithanya Eye Hospital & Research Institute consider Ocular oncology as a sub speciality which requires multimodal approach to provide comprehensive care. We believe in providing hope and striving our level best in conjunction with allied subspecialties to deal with the intricacies of eye tumours. Eye tumours can be divided vastly into extra ocular and intraocular tumours. Intraocular tumours can be of the anterior or posterior segment of the eye
WHY DO YOU NEED AN OCULAR ONCOLOGIST?
Ocular cancers are unique among the diseases of the eye, posing a threat to both vision and life. Most cases require a careful clinical history and specialized ocular examination. Ocular oncology diagnosis relies heavily on imaging techniques such as high-frequency Ultrasound, Fluorescein angiography, anterior and posterior segment Optical Coherence Tomography, Computed Tomography (CT), and Magnetic Resonance Imaging (MRI). Once we arrive at a diagnosis, treatment decisions depend on the tumour’s location, size, local extension, patterns of growth, and secondary complications. Treatment options include observation, local resection, chemotherapy (topical, intravenous, intra-arterial, or intravitreal), and radiation. Enucleation or exenteration is employed only if these eye- and vision-sparing treatments are not possible.
WHAT DO I NEED TO KNOW REGARDING ANTERIOR SEGMENT TUMOURS?
As we all know global atmospheric changes such as depletion of ozone in the stratosphere may lead to increased levels of ultraviolet radiation. As we live in the tropical climate UV radiation (both UV A and UV B) from the sun reaches you producing DNA changes that lead to skin cancers on the eyelid and conjunctival cancers once rare these eye cancers are increasing. It might surprise you to learn that basal cell carcinoma (BCC), squamous cell carcinoma (SCC) and melanoma on the eyelid can occur along with ocular surface squamous neoplasia.
WHAT DO I NEED TO KNOW REGARDING POSTERIOR SEGMENT TUMOURS?
While most cancers in man are more common well into adulthood, posterior segment eye tumours are most common in children and are associated with devastating ocular outcomes if not promptly identified and treated. Retinoblastoma is a malignant tumour of the retina, the light sensitive layer that lines the back of the eyes. Retinoblastoma is one of the most common solid tumors in infants and young children. However, most of them are diagnosed late only when they present with white appearance of the media of the eye (leukocoria), abnormal deviation of the eyeball (squint/strabismus), and rarely redness and an unusually prominent eyeball. These may be considered the “red flags” to consult the ocular oncologist for an urgent retinoblastoma screen in infancy and childhood. Periodic eye screen during well-baby visits helps in early diagnosis and referral to the ocular oncologist for timely management, and vision and eye salvage.
The ocular oncologist will evaluate the child by detailed eye examination under anesthesia. Advanced ultrasonographic scans and magnetic resonance imaging help in diagnosis and staging of the disease. Screening for extraocular spread may be required in advanced cases.
Around 40% of children with retinoblastoma have a hereditary form of the condition. Some children with hereditary retinoblastoma have inherited genetic mutation from a parent who had retinoblastoma as a child. Hereditary retinoblastoma usually develops at an earlier age and can involve both the eyes. Hereditary Retinoblastoma is also notorious to skip generations. Genetic evaluation holds significance in the management of Retinoblastoma. Individuals with abnormality in the RB-1 gene associated with retinoblastoma, are also at risk for developing cancers in other parts of the body later in life as well.
Ocular oncology services of Chaithanya Eye Hospital are poised to offer advanced treatment options for Retinoblastoma. Through a multidisciplinary team approach, these tumors can be managed with various forms of chemotherapy (intravenous, intraarterial, periocular and intravitreal), besides the surgical and radiation therapy options. We also offer advanced therapeutic modalities like cryotherapy and thermotherapy for vision and eye salvage. Our comprehensive ocular oncology services utilize the services of paediatric oncologist and interventional neuroradiologist.
Other tumours that can exist in the eye are nevus, melanoma, metastatic lesions, haemangioma, astrocytoma, lymphoma and leukemic infiltrates.
How do i make an appointment for this service?
For treatment for urgent and for a routine appointment with our consultants, you can come directly to, Chaithanya Eye Hospital & Research Institute and is working from Monday to Saturday, 9:00 am – 6:00 pm. For appointments call us at 0471 29 555 00 and our team shall confirm a date & time of your convenience based on the preferred consultant’s day and shall send across the confirmation to your registered mobile no/email, with us.
You can also get information and advice on eye conditions and treatments from our Video Consultation on +91 989 55 999 52. Staffed by experienced ophthalmic surgeons/consultants, the helpline is open from 9am to 6pm, Monday to Saturday. Busy times, we might not be able to answer your call straight away - please bear with us and call back a little later if this happens.
Do i need to bring someone with me?
We need to use eye drops to enlarge the pupil of the eyes for detailed posterior segment evaluation. These drops can blur your vision for between two and six hours. Thus, we advise that you bring someone along on the day of consultation to escort you. After dilatation you may not be able to drive a vehicle for up to 6 hours.
Trauma & Emergency Ophthalmic Services Department
Our Trauma & Emergency department aims to provide a first class service to people who have eye emergencies such as injury, pain or vision loss. The medical professional at our centre shall assess you upon your arrival to determine how serious your condition is and prioritize you accordingly.
Upon Arrival at Trauma & Emergency Care:-
Please fill in the form at the welcome kiosk and pass it over to the reception. The receptionist shall ask you some personal details so that they can register the patient details onto our system. And the patient will be assessed by our medical professional. This process helps us decide how urgent your eye problem is and how vital for you to be seen on the same day on a priority basis.
Please remember that the decision made about your treatment is based upon clinical expertise and your individual needs. Based on the initial assessment one of the following may happen:-
You will be examined by a nurse who will ask some questions, check your vision and carry of any relevant tests, after which you will be seen by our consultant and give you the appropriate treatment services.
You may be given appointment for the very next day for further detailed check up and treatment services.
You may be asked to return to Chaithanya Eye Hospital & Research Institute at a different date and time.
You may be told that there is no case of emergency treatment required.
PLEASE NOTE:-
Please be noted that patients are seen according to their clinical priority and not necessarily their time of arrival.
Patients with potentially contagious eye conditions will be asked to wait in a separate area.
Priority may be given to children, elderly and patients who are generally unwell, as they may need to be seen more urgently.
If you start feeling unwell while waiting, please inform our staff, who will ensure that you are assessed by our medical team and given the appropriate care.
If you have any further questions please do not hesitate to approach our staff – we are always happy to help.
General Ophthalmology Department

General Ophthalmology at Chaithanya Eye Hospital & Research Institute which is sometimes also known as primary care, provides a broad spectrum of eye care, from vision care to diagnosing and treating eye disease and those that might need referral to one of our more specialist service. Wide patients with a variety of symptoms and problems who range in age from new born child through elderly adults are seen by our consultants.
We at Chaithanya Eye Hospital and Research Institute, believes in seeing the eye as a whole. General ophthalmologist is the first doctor to see you and take care in diagnosing and treating various eye disorder. General Ophthalmologist will provide comprehensive eye check and refer you to specialists if need arises.
TREATMENT SERVICES AT CHAITHANYA
At our centre General Ophthalmology consultants are often the first consultants on our team to see patients for periodic medical eye exams and as well as for specific visual or ocular complaints. They take care of a variety of conditions such as diabetes, dry eye, etc.
The General Ophthalmology consultants at Chaithanya Eye Hospital & Research Institute evaluate a large range of symptoms such as blurry vision, poor night vision, transient loss of vision, loss of visual field, sudden loss of vision, difficulty with near vision, eye pain, red eyes, eye fatigue, fluctuating vision, itching or burring, crusts or discharge, excess tearing, double vision and itching or redness of eyelids.
Usually a full medical eye exam begins with a refraction, checking eye pressure, checking ocular alignment and motility and examining the anterior structures of the eye with a specialized slit lamp bio – microscope. A full examination often includes dilation of the pupils so that the posterior structure of the eye, such as the retina and optic nerve, can be examined.
General ophthalmology department clear mainly in:
Checking vision and prescribing spectacles.
Infective conditions of lids, adnexa, conjunctiva and cornea.
Injuries to the eye : Blunt injury, penetrating injury, chemical injuries
Allergic condition involving anterior segment of eye.
Evaluating and treating ocular causes of headache.
Other disorder of eye.
How do i make an appointment for this service?
For treatment for urgent and for a routine appointment with our Consultant, you can come directly to, Chaithanya Eye Hospital & Research Institute our working days are from Monday to Saturday, 9:00 am – 6:00 pm. For appointments call us at 0471 29 555 00 and our team shall confirm a date & time of your convenience based on the preferred consultant’s day and shall send across the confirmation to your registered mobile no/email, with us.
You can also get information and advice on eye conditions and treatments from our Video Consultation on +91 989 55 999 52. Staffed by experienced ophthalmic surgeons/consultants, the helpline is open from 9am to 6pm, Monday to Saturday. If our lines are busy, we might not be able to answer your call straight away - please bear with us and call back a little later if this happens.
DO I NEED TO BRING SOMEONE WITH ME ?
Occasionally we need to use eye drops to enlarge the pupil of the eyes so that we can examine the retina of the eye. These drops can blur your vision for around six hours or more. Thus we advise that you bring someone along on the day of consultation to escort you. After dilatation you may find it difficult to drive a vehicle for around 6 hours or more due to the induced glare.